JR Ryder et al. N Engl J Med 2024;391:1656-1658. DOI: 10.1056/NEJMc2404054. Ten-Year Outcomes after Bariatric Surgery in Adolescents
Methods: The Teen Longitudinal Assessment of Bariatric Surgery (Teen-LABS) is a prospective multicenter observational cohort study involving adolescents (13 to 19 years of age) undergoing bariatric surgery. Participating adolescents underwent either gastric bypass (161 participants) or sleeve gastrectomy (99 participants) at a mean age of 17 years. Overall, 83% of the 10-year postoperative visits were completed.
Key findings:
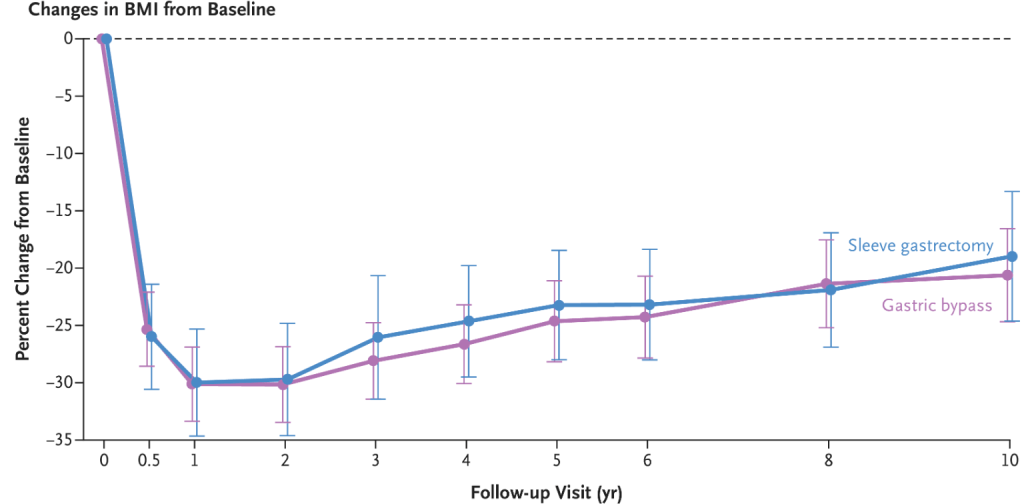
- The changes in BMI were similar with gastric bypass (mean change, −20.6%) and sleeve gastrectomy (mean change, −19.2%)
- Ten years after bariatric surgery, the modeled percentages of participants with remission of coexisting conditions (55% for type 2 diabetes, 57% for hypertension, and 54% for dyslipidemia)

My take (borrowed from authors): “These findings show the long-term durability of weight loss and remission of coexisting conditions after bariatric surgery, as well as the greater health benefits and durability of the effects in adolescents than would be expected in similarly treated adults.”
Related article: H Bliddal et al. N Engl J Med 2024;391:1573-1583. Once-Weekly Semaglutide in Persons with Obesity and Knee Osteoarthritis. Key finding: “treatment with once-weekly injectable semaglutide resulted in significantly greater reductions in body weight and pain related to knee osteoarthritis than placebo.”
Related blog posts:
- Adolescent Bariatric Outcomes
- Bariatric Surgery Outcomes in Adolescents
- How Many Kids Would Be Good Candidates for Bariatric Surgery?
- 12 Year Data: Pros and Cons with Bariatric Surgery
- Bariatric Surgery Reduced Obesity’s Premature Death from 8 years to 5 years in SOS Study
- Getting over the Stigma of Medicines for Anxiety/Depression and Obesity
- Meds for Obesity: AAP Guidelines
- NY Times: Bariatric Surgery at 16
- Nutritional Risks in Adolescents After Bariatric Surgery; Prevention of Childhood Obesity; Convalescent Serum for COVID-19
- GLP-1 Obesity Medication for 6-11 Year Olds
- Primary Prevention of Obesity Still Needed

