N Ravanbakhsh et al J Pediatr Gastroenterol Nutr. 2024;79:1192–1198. Comparing imaging modalities in the assessment of fibrosis in metabolic dysfunction-associated steatotic liver disease
In this retrospective review with 77 patients who had liver biopsy-proven MASLD (2017-2023), the authors examined how well magnetic resonance elastoraphy (MRE) and transient elastography (TE) identified fibrosis.
Key findings:
- Fibrosis was identified in 90% of liver biopsies
- The area under the receiver operating characteristic curves (AUROC) of MRE and TE for detection of high-grade fibrosis were 0.817 and 0.750, respectively
- Only 20% of patients had severe fibrosis on liver biopsy; thus, this is a limitation given the small number
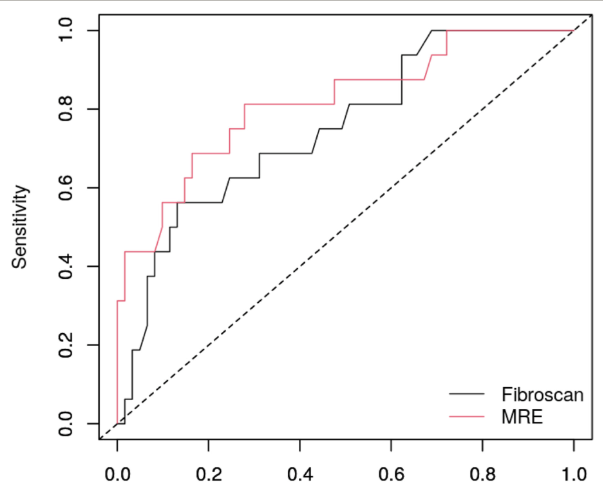
Conclusion of authors: “MRE and TE did not accurately predict high-grade fibrosis on liver biopsy. Between the two noninvasive imaging modalities, the correlation of identifying high-grade fibrosis was not statistically different.”
My take: Even MRE is not very accurate at identifying fibrosis. Given the huge numbers of individuals (pediatric and adult) with MASLD, the lack of reliable non-invasive markers is a problematic. As effective treatments become available, being able to determine if they are working is essential.
Related blog posts:
- AASLD Practice Changes for Metabolic Liver Disease in 2024
- Resmetirom for MASH
- Three-fer on Steatotic Liver Disease
- Fibrosis and Steatotic Liver Disease -Who Needs to be Followed by Hepatology?
- Prevalence of Steatotic Liver Disease in U.S. And Risk of Complications
- How Many Kids Would Be Good Candidates for Bariatric Surgery?
- You No Longer Have Fatty Liver Disease-You Have Steatotic Liver Disease!
- Transient Elastography in Pediatric Liver Disease
- Magnetic Resonance Elastography in Nonalcoholic Fatty Liver Disease