R Mandile et al. J Pediatr Gastroenterol Nutr. 2025;81:1482–1487. Advantages of anti-endomysial evaluation in children with low titers of anti-transglutaminase antibodies: A retrospective study
This was a single center retrospective study examining children (n=202) undergoing EGD (2022-2024) to evaluate for celiac. Among those with low anti-TTG IgA titers, Group 1 (n=25) was EMA negative and Group 2 (n=100) was EMA positive.
Key findings:
- The finding of discordant serology (anti-transglutaminase [anti-TG] positive and EMA negative) is infrequent (12% cases, 25 out of 202), and all patients with discordant serology had anti-TG positive at low titer (<4 times the upper limit of normality).
- Group 1 (N = 25) had a mean anti-TG titer of 1.86× ULN and villous atrophy (VA) in only 8% (2/25). Group 2 (N = 100) had VA in 35% (35/100)

Discussion Points:
- The diagnosis of CD still requires performing an EGD in at least half of the cases
- This “study suggests that patients with low levels of anti-TG but EMA positive antibodies should anyway receive an EGDS in the next 6 months, since in around one-third of the cases a duodenal atrophy will be detected”
- In those with low anti-TG but EMA negative, ” it could be reasonable to initially follow-up patients over time with clinical and serological monitoring (in particular of anti-TG titer), postponing the EGDS to a later stage, when the disease is more advanced and the chance of finding a concomitant VA (and thus the need to start a GFD) is higher”
My take: In patients with minimal symptoms and low level anti-TG, my strategy has been to follow with serological monitoring and if repeatedly abnormal, proceed with endoscopy. This study suggests that obtaining EMA early may influence choice to proceed earlier with endoscopy.
Related blog posts
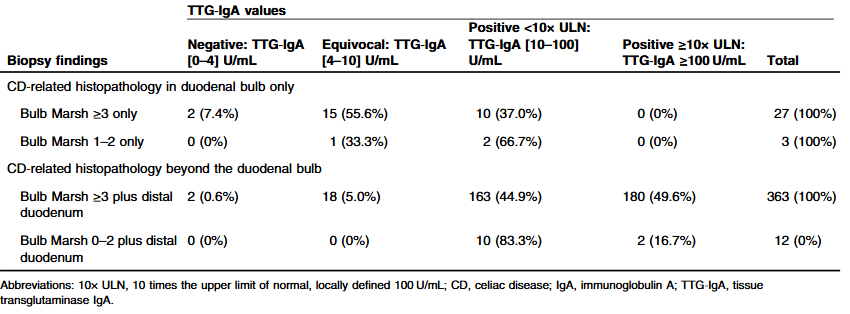
- Celiac Disease: Lower TTG-IgA Titers Associated with Isolated Duodenal Bulb Presentation
- Shared Decision-Making in Celiac Disease Diagnostic Approach
- When Celiac Disease Symptoms Continue Despite a Gluten Free Diet:
- New Data on the Reliability of the No-Biopsy Diagnosis in Pediatric Celiac Disease
- Immune Dysregulation Can Mimic Celiac Disease
- Celiac Risk Among First-Degree Relatives of Index Case
- Dr. Arun Singh: Tips and Tricks to Managing Celiac Disease
- Safe for Patients with Celiac Disease to Kiss after Partner’s Gluten Ingestion
- Clever Study to Assess Utility of TTG IgA For Monitoring Response to a Gluten-Free Diet