S Wu et al. Clin Gastroenterol Hepatol 2024; 22: 1497-1507. Ultra-Processed Food Consumption and Long-Term Risk of Irritable Bowel Syndrome: A Large-Scale Prospective Cohort Study
Methods: Participants (N = 178,711) who completed 24-hour dietary recalls during 2009 to 2012 from the UK Biobank, and free of IBS, celiac disease, inflammatory bowel disease, and any cancer at baseline, were included. During a median of 11.3 years of follow-up, 2690 incident IBS cases were identified.
Key findings:
- The mean UPF consumption was 21.0% (SD, 11.0%) of the total diet
- An 8% higher risk of IBS (hazard ratio, 1.08; 95% CI, 1.04–1.12) was associated with every 10% increment of UPF consumption
- Compared with the lowest quartile of UPF consumption, the highest quartile was associated with a significantly increased risk of incident IBS (hazard ratio, 1.19)
Discussion:
- “The worsening global epidemic of IBS has coincided with increased dietary consumption of UPF over the past few decades…A similar positive association with IBS (odds ratio of quartile 4 vs quartile 1 = 1.25; 95% CI, 1.12–1.39) was detected in…the French NutriNet-Santé study”
- High UPF consumption has been associated with “a 42% greater risk of nonalcoholic fatty liver disease and a 22% greater risk of depression.”
- The authors note that with an observational study, this limits the determination of causality between UPF and IBS
My take: Yet, another study showing that UPF are associated with negative health outcomes. This study reported that UPF consumption was 21% of participants’ diet. In U.S., the current estimate is 60-70% (Source: NPR May 2023: What we know about the health risks of ultra-processed foods). It would be helpful if these foods that are bad for our health did not taste so good!
Related blog posts:
- More Data Supporting Dietary Treatment for Irritable Bowel
- Which Diet is Best for Irritable Bowel Syndrome? A Randomized Trial
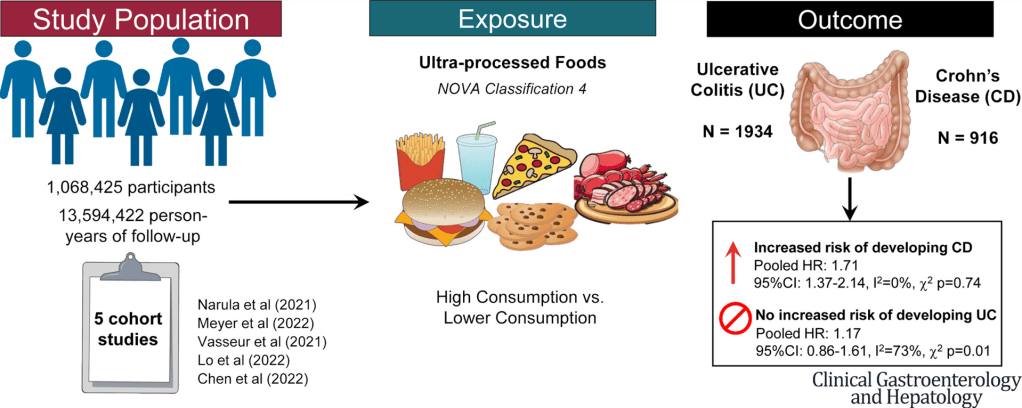
- Ultraprocessed Food and the Risk of Inflammatory Bowel Disease
- What is Mild Crohn’s Disease and How to Treat It
- AGA Guidance: Nutritional Therapies for Inflammatory Bowel Disease
- Risk Factors for Inflammatory Bowel Disease: Ultra-Processed Food (Part 1)
- Call For Action: Adolescent Nutrition Series
- “The Paramount Health Challenge for Humans in the 21st Century”
- NY Times: “Our Food is Killing Too Many of Us”