Danielle Ofri, NY Times 7/28/25: Doctors Have Lost Their Mount Olympus of Medicine
This entire essay is worth reading but may be behind a paywall.
An excerpt:
For most of my colleagues and me, the C.D.C. and the N.I.H. were the medical Mount Olympus, the towering pillars of medical authority. Contrary to right-wing portrayals, these were not dictatorial authorities. These were earned authorities, comprising our best, brightest and most dedicated peers. The formidable talents of these doctors and scientists would have commanded enviable salaries had they taken jobs in industry, but they chose the public sector instead — something that we clinicians were forever grateful for…
While there are some doctors who viewed our public health institutions with disdain — some of them now are running these very organizations — most practicing physicians relied heavily on them to deliver the best care possible to their patients, despite occasional quibbles. What a relief, I always felt, that there were people organizing the things I can’t do — testing new treatments, conducting population studies, keeping tabs on worldwide diseases, issuing guidelines and more.
But now that support is a shell of what it once was. I can no longer automatically rely on these institutions because their scientific North Star, even if imperfect at times, has been replaced by one that seems nakedly political. Remaining staffs are no doubt working valiantly to do their jobs, but they are hobbled by loss of colleagues, resources and reliable leadership. So when I hear that the C.D.C. has changed a vaccine recommendation, I now question whether that’s a recommendation I can trust. When the F.D.A. commissioner says he wants to change how the agency approves or rejects new treatments, I no longer feel sure that science is driving those decisions. It’s hard to convey how profoundly grieved my colleagues and I feel…
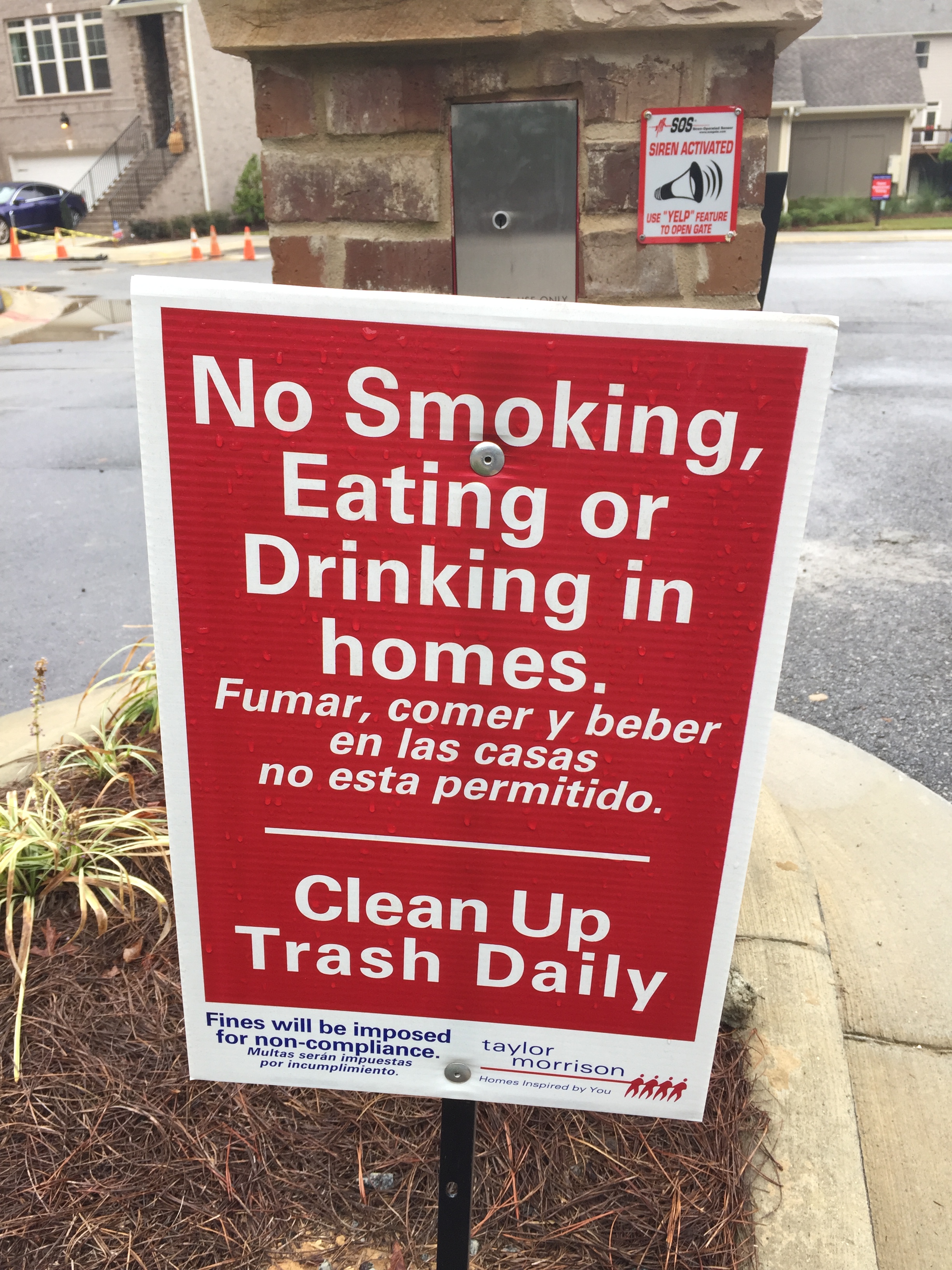
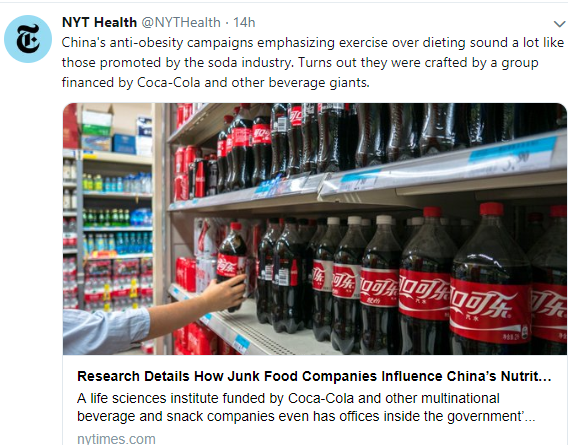
Robert F. Kennedy Jr.’s view seems to be that we doctors are shills for corporate interests and government bureaucrats, and that torching our vaunted institutions is the prescription to fix us. Mr. Kennedy’s ire seems oddly directed. I, too, am disgusted by the role of money in health care, but I see it more as a result of the system we’ve set up, rather than the people who labor within it…
Notably missing from Mr. Kennedy’s Make America Healthy Again agenda is any suggestion that we provide universal health care, as most other developed countries do. There is no push to expand Medicare and Medicaid, which help some of our sickest patients. There is no focus on expanding access to early childhood education and supplemental nutrition programs, which offer steep health benefits…[There] is a barely concealed antipathy toward the people who are the engine of these institutions — doctors, scientists, policy wonks…
Cuts to infectious-disease surveillance means that outbreaks will almost certainly creep up more stealthily on our patients. Cuts to the National Center for Chronic Disease Prevention and Health Promotion means fewer resources for prevention of cancer, heart disease and diabetes — some of the leading causes of death. Cuts to the N.I.H and the F.D.A. could drastically reduce the development and approval of new medical treatments. Add in cuts to injury-prevention research and patient safety programs, and it’s a prescription to make America sick again.
Every time you go to your doctor or get treated by a nurse, there’s a chorus of researchers, public health workers, policy experts, epidemiologists and advisory panels arrayed behind them, aided by laboratories, databases, websites, early-detection systems and clinical guidelines. Our current government seems determined to wrench this away, handicapping your health care team’s ability to care for you.
My take (borrowed in part from author): Our health care system needs to improve costs, accessibility, and outcomes. Yet, the changes to our healthcare and research under this administration are making matters worse. “So many of our resources are now gone, and those that remain no longer feel trustworthy. Americans’ health will decline at the hands of our federal government. And there’s no vaccine for that.”
Related blog posts:
- RFK Jr. Ousts Entire CDC Vaccine Advisory Committee
- “How to Make America Healthy: the Real Problems — and Best Fixes”
- “Optimal dietary patterns for healthy aging”
- Calamitous Impact of U.S. Withdrawal from Gavi Funding
- Longevity Gap Present Even in Wealthy Americans
- Ten Americas: Examining Health Disparities and Life Expectancy
- How Putting America First is Undermining Health Outcomes Here and Globally
- No Exaggeration: Too Many Children Are Dying in the U.S.
- Firearms: #1 Cause of Pediatric Deaths & Households with Guns =More Deaths