H Gagnon et al. JPGN 2023; 77: 592-596. Short and Long-Term Outcomes in Hirschsprung Disease: Are the Syndrome-Associated Patients Really Doing Worse?
In this retrospective single-center study with 76 pediatric patients with Hirschsprung’s disease (HD), the authors compared the outcomes of those who had associated syndromes (or neurocognitive issues) (SA-HD, n=24) to those with isolated (I-HD, n=52). Most patients had undergone a Soave procedure (n=67). Only 11 patients were available for followup data at 10 years of age.
Key findings:
- SA-HD patients became bowel continent at a significantly older age (mean age 8.43 vs 4.94 years)
- SA-HD patients had urinary incontinence at a significantly older age (P = 0.0136, 5 years)
- SA-HD patients had more constipation at all ages: at age 3 years (29% vs 17%), at age 5 years (55% vs 22%), and at 10 years (83% vs 20%)
- SA-HD included Down syndrome (38%), cognitive impairment (29%), MEN (8%), hypoventilation syndrome (aka Ondine) (8%), oro-facio-digital (8%), Smith-Lemli-Opitz (4%) and Bardet-Biedl (4%). The authors note that expected toilet training completion for Down syndrome is between 4.7-6.6 years of age compared to 2.3-3.4 years for neurotypical kids.
My take: Since SA-HD includes children with high rates of cognitive impairment, it is not surprising that there were delays in toilet training, higher rates of constipation and higher rates of urinary retention.
The study reinforces the need for long-term follow-up in this cohort. NASPGHAN has provided a useful position paper (JPGN 2023; 76: 533-546. Open Access! Evaluation and Management of Postsurgical Patient With Hirschsprung Disease Neurogastroenterology & Motility Committee: Position Paper of North American Society of Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN)).
Related blog posts:
- Good Bowel Sound Podcasts: Cow’s Milk Intolerance and Hirschspurng Disease
- You Can Do Anorectal Manometry in Your Sleep, But Should You?
- Reducing Diagnostic Uncertainty in Hirschsprung’s Disease
- Work on Both Ends
- Image Only: Total Colonic Aganglionosis
- Rectal Suction Biopsies Less Accurate in Infants <40 days
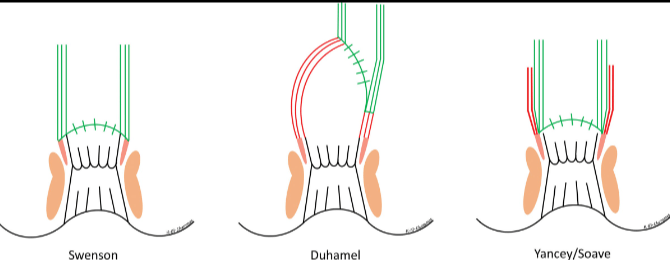
From left to right: full-thickness rectosigmoid dissection (Swenson), a recto-rectal pouch procedure (Duhamel), and an endorectal dissection (Soave). JPGN 2023; 76(4):533-546.