M Allocca et al. Gastroenterol 2023; 164: 851-855. Open Access! Intestinal Ultrasound in the Assessment and Management of Inflammatory Bowel Disease: Is It Ready for Standard Practice?
This short article outlines the indications, availability, technical skills, cost-effectiveness and potential value of intestinal ultrasound (IUS). Some key points:
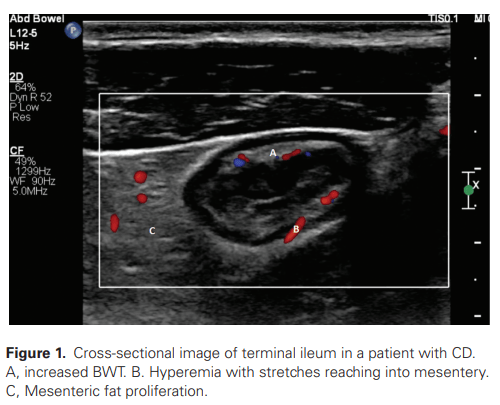
- Goal: “IUS is used as a first-line investigation and can avoid or delay the need for more invasive and expensive testing (CT, MRI, or colonoscopy). Thus, costs are minimized and patient convenience is optimized”
- Availability: “IUS is quite widespread in many European countries, but its uptake has been significantly less in other parts of the world, including the United States. Limitations to its use include the absence of standardized and reproducible protocols, lack of local expertise, and the perception that IUS is an operator-dependent tool, feasible only by highly experienced operators. In reality, however,…. studies specifically addressing sonographer variability demonstrate substantial agreement for color Doppler signals and almost perfect agreement for bowel-wall thickness, as the most relevant IUS parameter.”
- Expertise: Trainees “have to perform at least 300 supervised ultrasound examinations in Italy and 400 in Germany to achieve full competency…It is believed that learners can achieve competency in IUS after approximately 200 supervised examinations, but it is important to acknowledge that a formal learning curve and the criteria for competency assessment have not yet been fully defined”
My take: Despite all the interest in this useful point-of-care tool, for IUS to become more widespread in the U.S. it will need to be incorporated in training programs. The threshold for competency is not achievable with a weekend seminar. It will be interesting to see how this test affects cost, management, and outcomes. Will it reduce or increase other cross sectional imaging testing? Is the information from IUS more useful than a calprotectin (stool biomarker) which could also be a point-of-care test?
Related blog posts:
- How Does Bowel Ultrasound Stack Up to MRE for Crohn’s Disease?
- Coming to a GI Clinic Near You? Intestinal Ultrasound for Ulcerative Colitis
- IBD Updates: Understanding Newest IBD Therapies for Kids- Bowel Sounds, Hispanic Patients with IBD, More on Intestinal Ultrasound


The Oro Valley/Tucson Loop shared use bike path extends over 130 car free miles throughout unincorporated Pima County, Marana, Oro Valley, and Tucson.