K Chen et al. Inflamm Bowel Dis 2023; 29: 1499-1503. Serum Ustekinumab Concentrations Are Associated With Improved Outcomes With the Magnetic Resonance Index of Activity for Crohn’s Disease
This retrospective trial included thirty three patients with Crohn’s disease (CD) receiving maintenance ustekinumab (UST). The simplified Magnetic Resonance Index of Activity (sMARIA) and biomarkers were correlated with UST levels. The authors utilized a homologous mobility shift assay (HMSA) (Prometheus) for their UST levels.
Key findings:
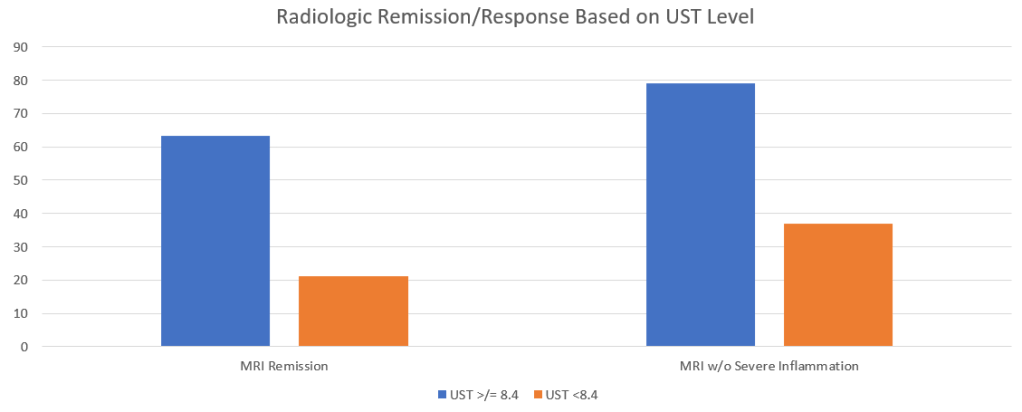
Both findings were clinically-significant P=.01
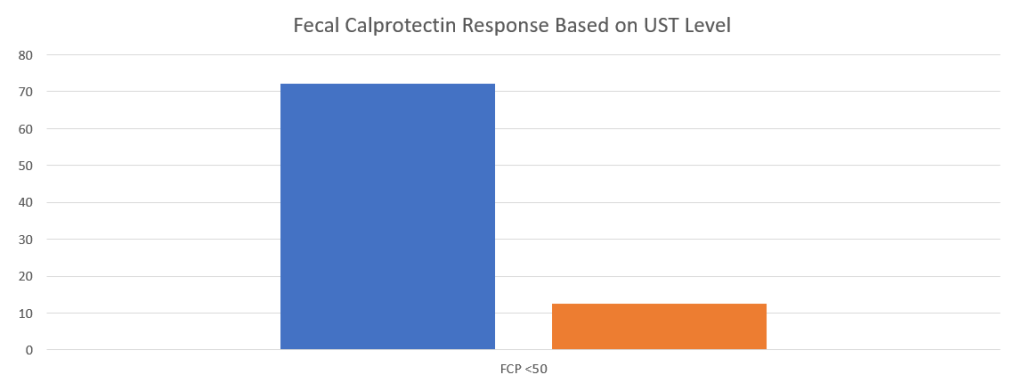
My take: This study show the need for higher levels of UST to achieve optimal outcomes. Levels of at least 8.4 appear to be a good target.
Related blog posts:
- Head-to-Head (Sort of): Infliximab vs Ustekinumab for Crohn’s Disease
- Dose Escalation of Ustekinumab & Support Tool “Should I Have IBD Surgery?”
- Can You Give Ustekinumab Subcutaneously After IV Reaction?
- Ustekinumab Escalation in Patients with Crohn’s Disease & Healthy Lifestyle Choices for IBD Patients
- CCFA 2023 (Atlanta) -Part 1
- CCFA 2023 (Atlanta) Part 4
- Therapeutic Drug Monitoring: Ustekinumab (Stelara) (In 2017, this study suggested a level of at least 4.5)
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.