DR Duncan et al. J Pediatr 2024; 272: 114128. Brief Resolved Unexplained Events Symptoms Frequently Result in Inappropriate Gastrointestinal Diagnoses and Treatment
In this prospective cohort study from Boston Children’s (2017-2022, n=157), the authors examined diagnostic evaluations in children presenting with Brief Resolved Unexplained Events (BRUEs).
Key findings:
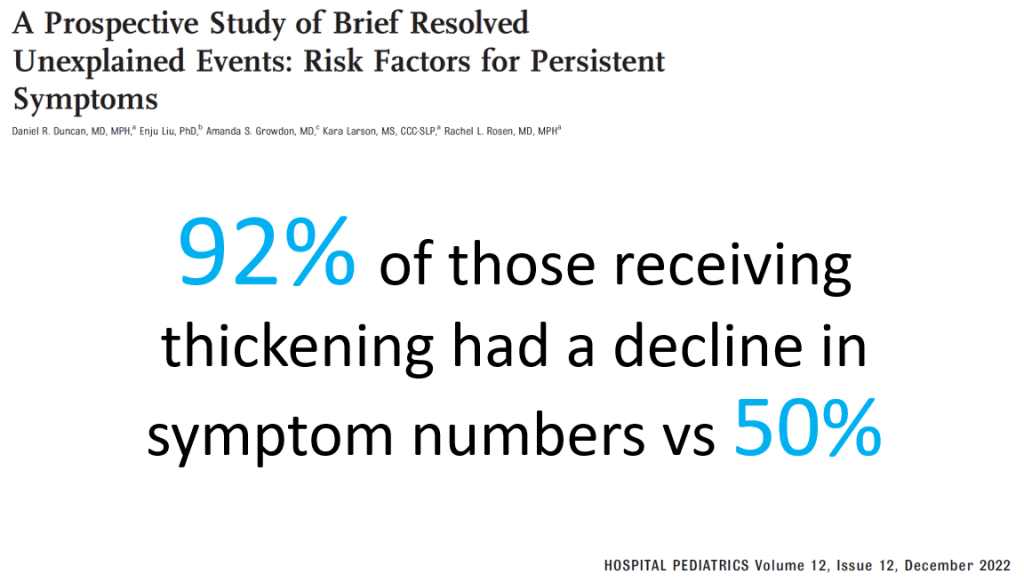
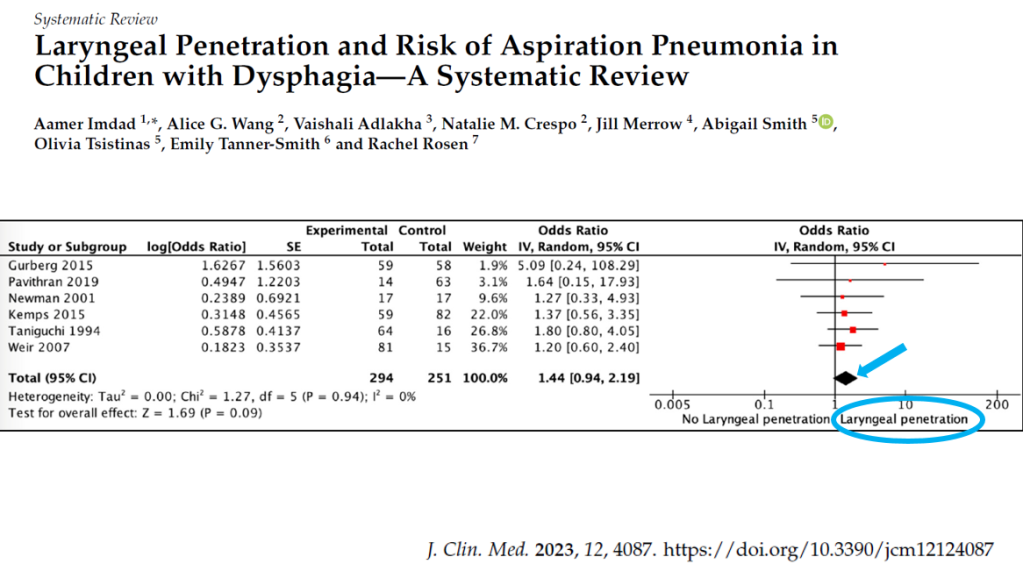
- Only 28% (20% during the hospitalization, 8% afterwards) underwent VFSS with 71% abnormal.
- 42% of infants had their BRUE attributed to GERD, and 33% were treated with acid suppression during follow-up
- Provision of GERD diagnosis was associated with a delay in making an aspiration diagnosis. 10% (6/66) of patients with “GERD” diagnosis subsequently had swallow studies –all were abnormal. Mean diagnostic delay was 56 days.
Discussion points:
- The approach of using symptoms to determine evaluation of BRUEs has been advised by AAP clinical practice guidelines (2016 & 2019); “however, our results suggest that reliance on these clinical characteristics may result in negative outcomes.”
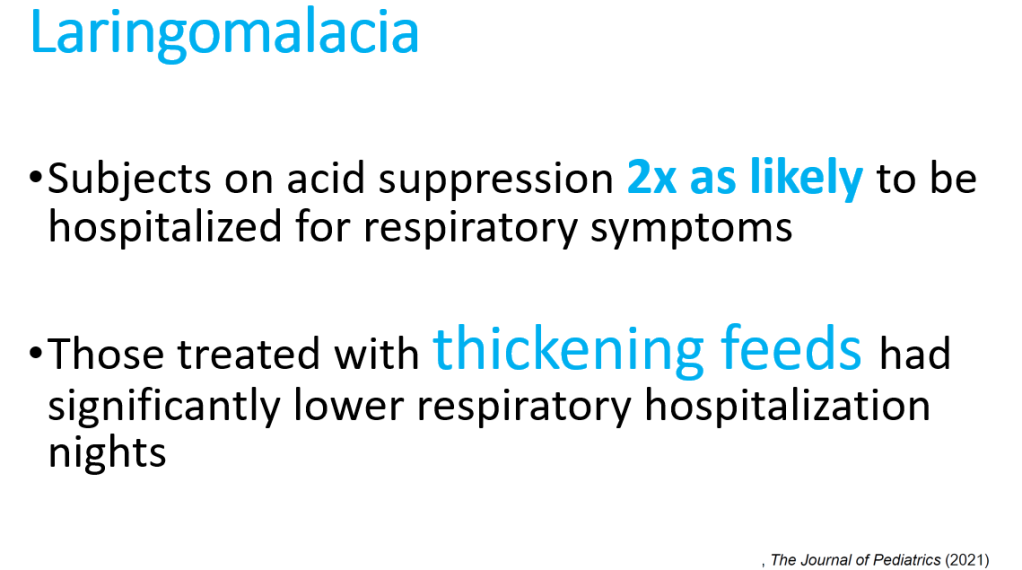
- Most aspiration in infants is silent aspiration and not detected by clinical feeding evaluation (CFE) in the absence of a VFSS. “It is concerning that 63% of patients had CFE alone without confirmatory VFSS in the present cohort, and it may be that this practice is even more common in other centers.” Silent aspiration can lead to repeat hospital visits and even long-lasting pulmonary damage including bronchiectasis.
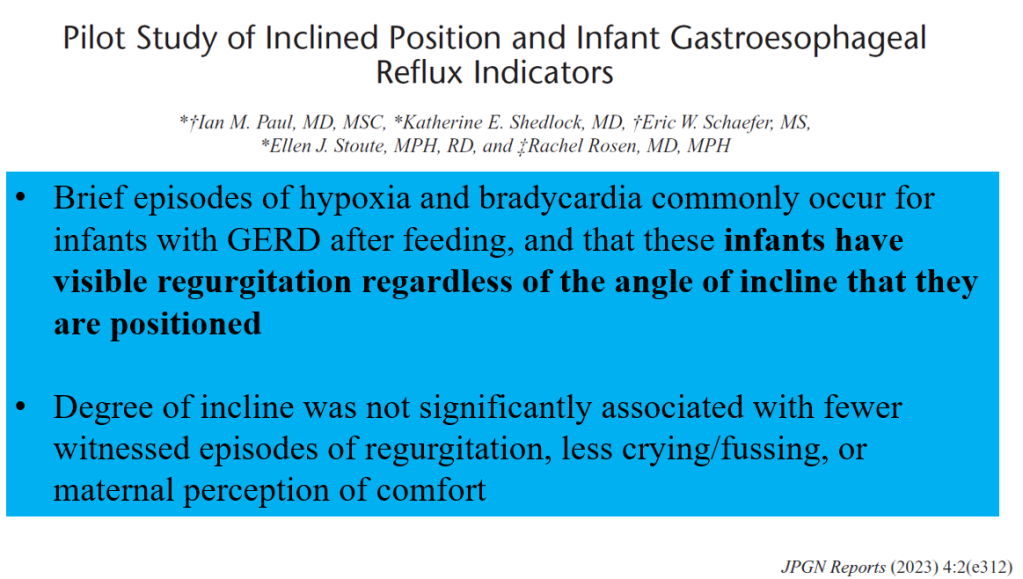
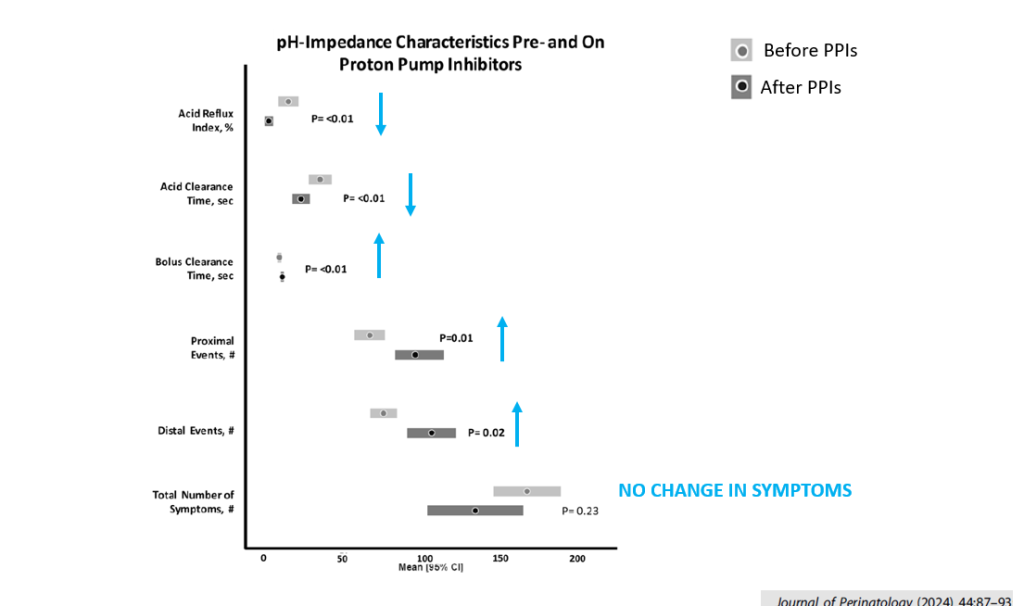
- Establishing a GERD diagnosis likely increases unnecessary (& potentially harmful) acid suppression
My take: The two punches in this study:
- Clinicians cannot diagnose aspiration based on history or bedside feeding evaluations. Objective testing (e.g. VFSS) is needed if there are concerns for dysphagia
- Inappropriate diagnosis of GERD may cause harm. GERD medications have been associated with increased infections and may increase risk for allergies.
The role of aspiration in causing BRUEs has been well-recognized since 2017 (see below) by the same group in Boston. It is likely that evaluation of dysphagia is even less frequent in other medical centers.
Related blog posts:
- Arching in Infants Not Due to Reflux
- Incredible Review of GERD, BRUE, Aspiration, and Gastroparesis
- Blaming Reflux for BRUEs -Not Changing Despite Guideline Recommendations (2019)
- Something Useful for ALTEs (BRUEs) (2017)
- 2018 AAP: Reflux Management in Preterm Infants
- 2018 Pediatric Gastroesophageal Reflux Guidelines
- How Many Kids with Reflux have Reflux?