The NASPGHAN Endoscopy Committee has published a very helpful “Management of Ingested Foreign Bodies” Report (Kramer RE et al. JPGN 2015; 60: 562-74). At the current time, one way to access a PDF of the report is the following CME link on the NASPGHAN website (no login required): Management of Ingested Foreign Bodies -Clinical Report
Some key definitiions from the report.
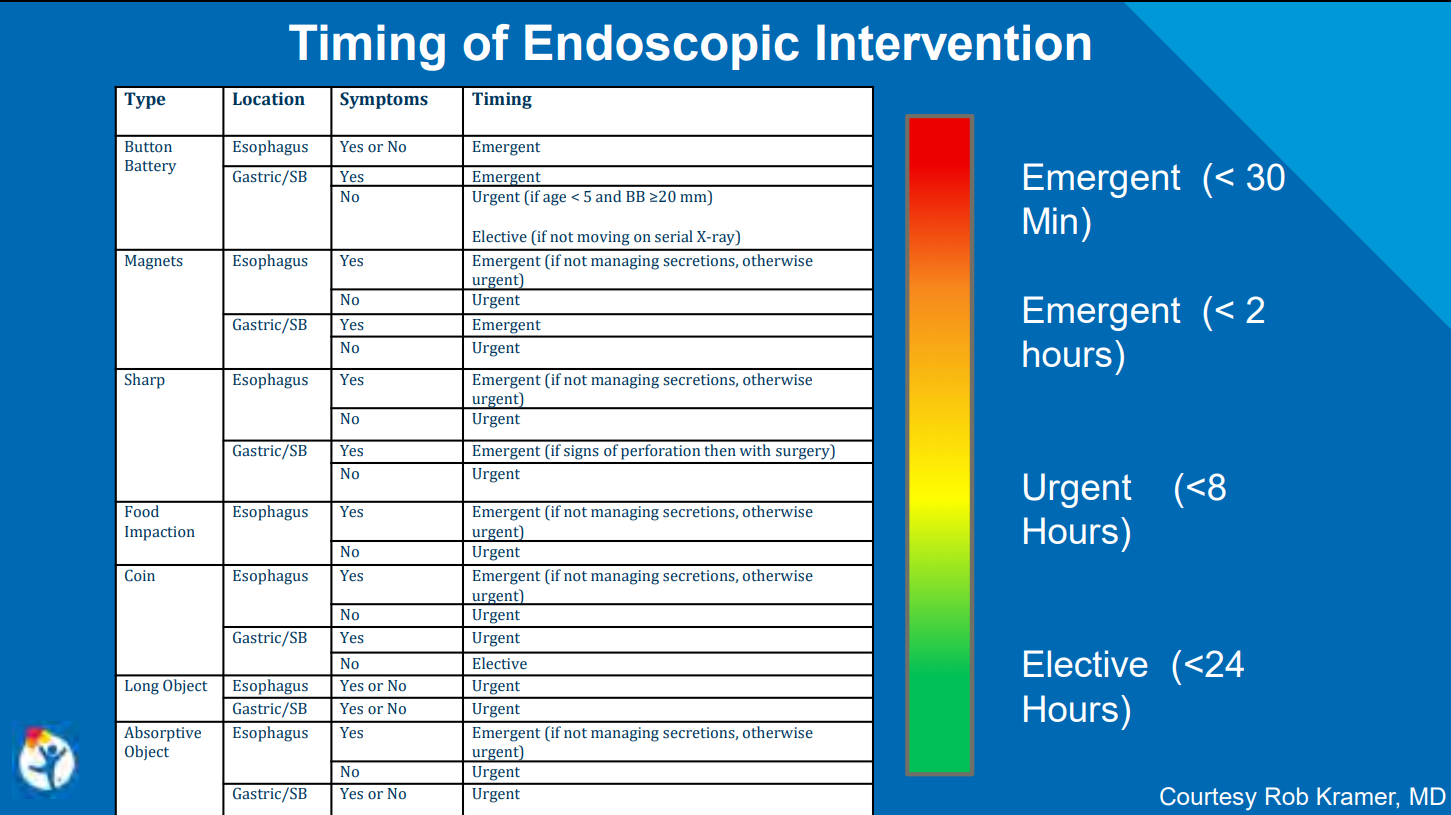
- Emergent removal <2 hours from presentation regardless of NPO status
- Urgent removal <24 hours from presentation following usual NPO guidelines
As a general rule, all symptomatic ingestions in the esophagus require emergent removal if feasible. Most gastric ingestions do not require emergent removal, exceptions include multiple magnets, sharp objects in stomach (possibly with surgery), and possibly absorptive objects (due to obstruction).
1. Button Batteries:
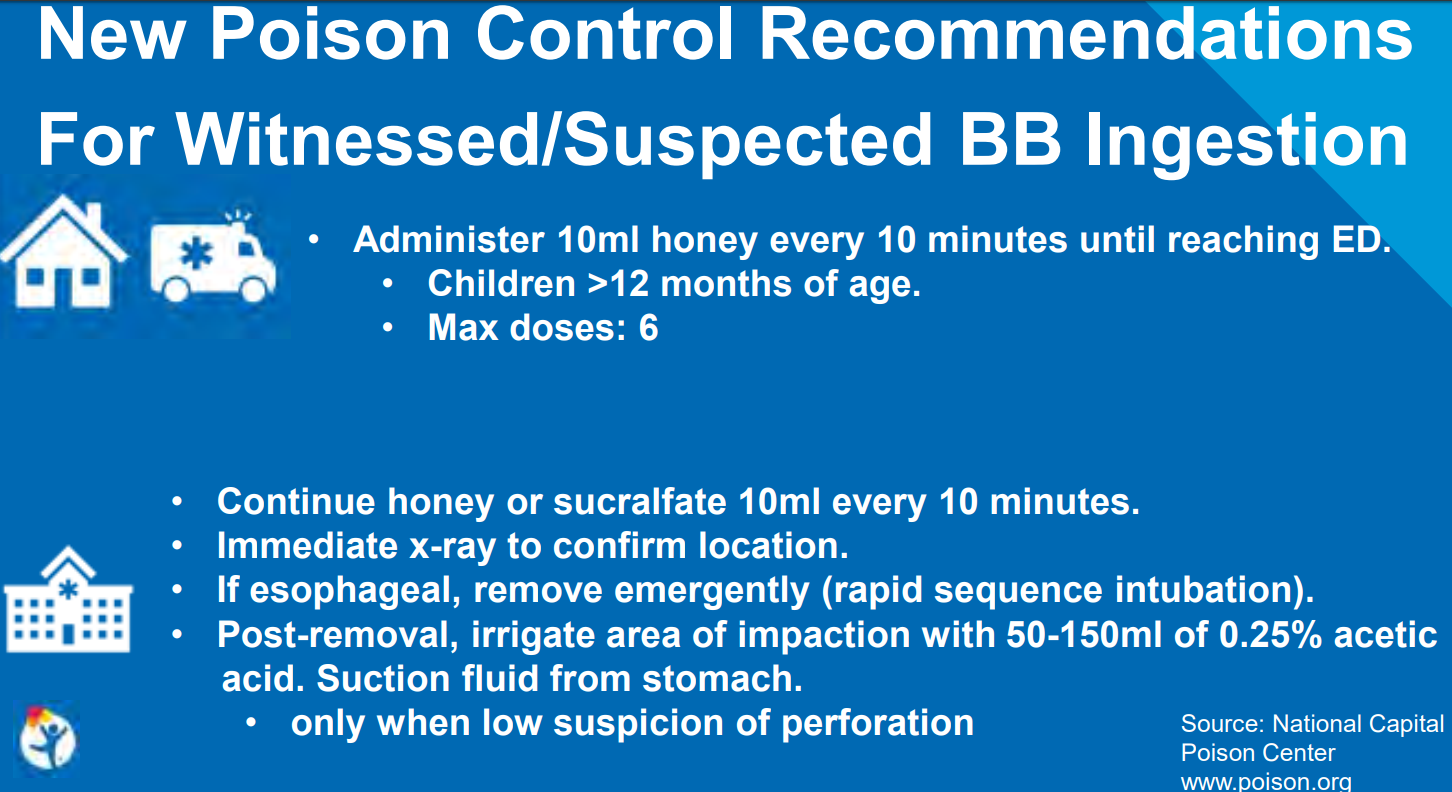
- Even with “spent” batteries, there is enough residual charge to cause injury and all ingestions (even if asymptomatic) into the esophagus require emergent removal. If these batteries are in the stomach & asymptomatic, urgent removal is recommended if age < 5 years and BB ≥20 mm.
What is different in the proposed algorithm (Figure 1) compared with the Poison Center Guidelines (see:Button Battery Algorithm Link | gutsandgrowth) is more detail regarding concerns about aortoenteric fistula & what to do after endoscopy. Key points:
- If active bleeding or unstable, endoscopic removal in OR with surgery/cardiovascular surgery is recommended.
- If any esophageal injury, recommendations include admission, NPO, and IV antibiotics. Chest imaging (CT angiography &/or MRI of chest) can help decide length of stay. In those with injury close to aorta, continuation of NPO/antibiotics are recommended along with followup imaging every 5-7 days. In those with clinical deterioration (eg. hematemesis w/in 21 days of injury), ‘assume aortoenteric fistula and emergently prepare for cardiovascular surgery.’
2. Magnets. Figure 3 provides algorithm for single and multiple magnets (adapted from Hussain SZ et al. JPGN 2012; 55: 239-42).
- For single magnets, emergent removal from esophagus is recommended (like all other foreign bodies) if difficulty managing secretions, otherwise urgent esophageal removal is suggested.
- If there are multiple magnets within reach of endoscope, then if symptomatic, emergent removal is recommended, otherwise, urgent removal is suggested.
- For asymptomatic magnets beyond the reach of an upper endoscopy, potential for colonoscopy, or enteroscopy for removal &/or serial x-rays to follow progression. If there is no progression on X-rays (every 8-12 hrs) &/or development of symptoms, then surgical removal/endoscopic removal is recommended.
3. Sharp objects. Figure 4 provides algorithm.
- Emergent removal from esophagus/stomach is recommended (like all other foreign bodies) if difficulty managing secretions, otherwise urgent esophageal removal is suggested. For radiolucent objects, if the ingestion was witnessed, urgent removal is suggested; if not witnessed, then further imaging (CT, esophagram, MRI) could be considered.
- With regard to sharp foreign bodies beyond the reach of an endoscope, “follow clinically with serial x-ray. Enteroscopy or surgical removal considered if symptoms develop or >3 days without passage.”
- Despite the low risk of severe morbidity/mortality from sharp objects (beyond esophagus), report recommends urgent “removal of all of the sharp objects within the reach of the endoscope..if possible.”
4. Food impaction in esophagus. If symptomatic, emergent removal; if asymptomatic, then urgent removal. Biopsies of the esophagus are recommended with endoscopy (Figure 5).
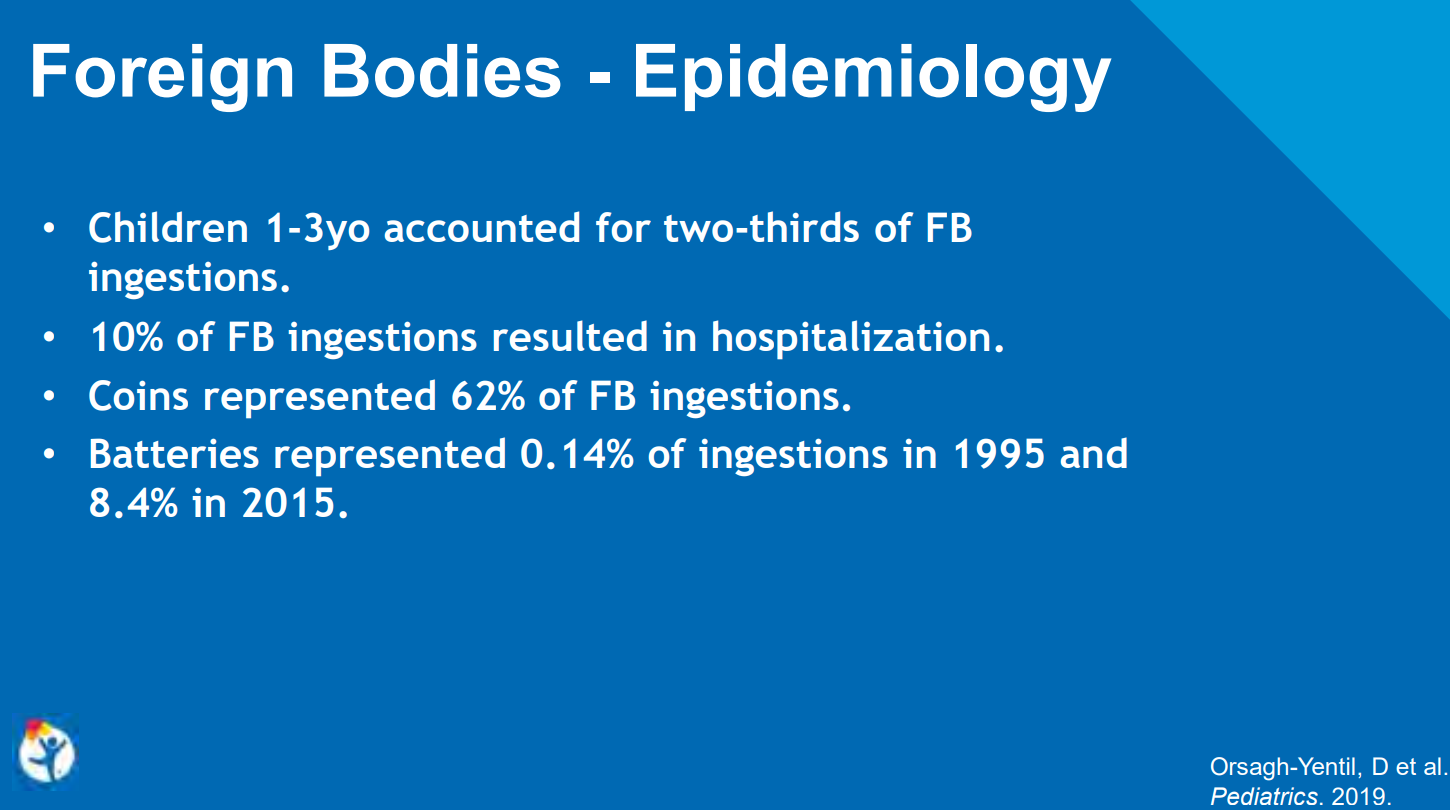
5. Coin ingestions/Blunt objects. Figure 6. “>250,000 ingestions and 20 deaths reported in the United States during a 10-year period.”
- For esophagus: If symptomatic, emergent removal; if asymptomatic, then urgent removal. Report recommends check X-ray immediately before sedation. While the report does not address this, a possible alternative to x-ray would be the use of a metal detector. “Consider glucagon if distal esophageal coin or if endoscopy not readily available.”
- For stomach: No endoscopy needed. Repeat X-ray at 2 weeks. Remove if not passed w/in 2-4 weeks. Report recommends check X-ray immediately before sedation. While the report does not address this, a possible alternative to x-ray would be the use of a metal detector.
- For small bowel: removal (enteroscopy/surgery) if symptomatic.
- For objects >25 mm width or >6 cm in length –> should be removed from stomach urgently.
6. Superabsorbent objects. The authors describe ingestions from materials from toys and diapers with polymers that can retain ‘up to 100 times their weight in water.”
- For esophagus: If symptomatic, emergent removal; if asymptomatic, then urgent removal.
- Stomach/small intestine: urgent removal is recommended
The authors state these recommendations are based on consensus rather than strong evidence and are “no substitute for clinical judgement.”
Take-home message: These guidelines are a good starting point to improve the management of children with foreign bodies.
Related blog posts:
Disclaimer: These blog posts are for educational purposes only. Specific dosing of medications/diets (along with potential adverse effects) should be confirmed by prescribing physician/nutritionist. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.

University of Chicago