S Singh et al. Gastroenterol 2023; 164: 344-372. Open Access! AGA Clinical Practice Guideline on the Role of Biomarkers for the Management of Ulcerative Colitis Clinical Decision support tool (pg 373-374), Spotlight (pg 375).
The full access links to the article and related articles provide extensive information and rationale for AGA’s biomarker recommendations in ulcerative colitis (UC). For me, the recommendations highlight the important role of biomarkers (especially fecal calprotectin (FC)) when things are going very well or very poorly. Key points:
- In asymptomatic patients with normal biomarkers (FC <150, normal lactoferrin, normal CRP), the recommendations suggest continued monitoring without endoscopic assessment.
- In patients with moderate-to-severe symptoms and with elevated biomarkers, the authors, likewise, advocate for treatment adjustment without endoscopic assessment.
- For asymptomatic patients with elevated biomarkers and symptomatic patients with normal biomarkers, the authors recommend endoscopic assessment.
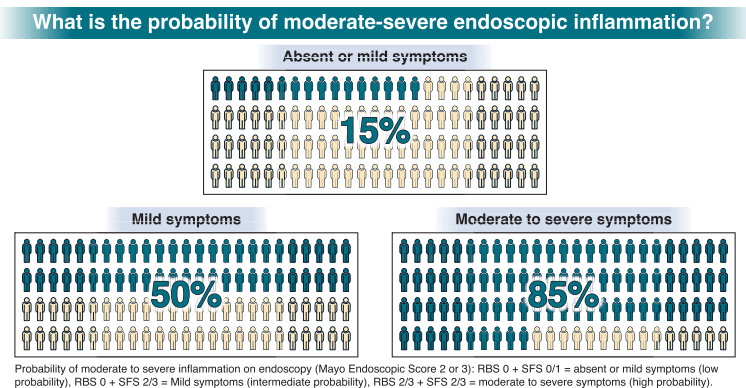
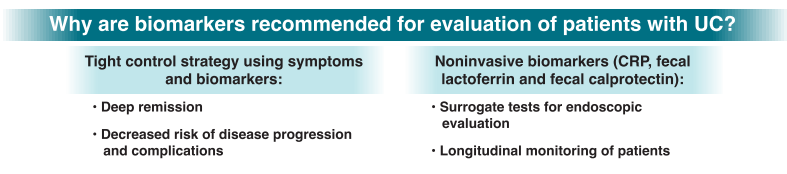
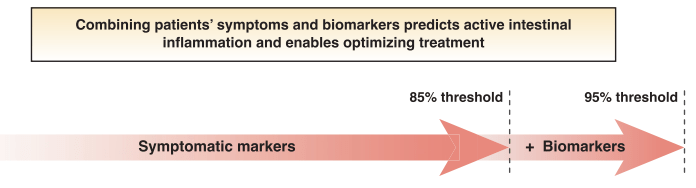
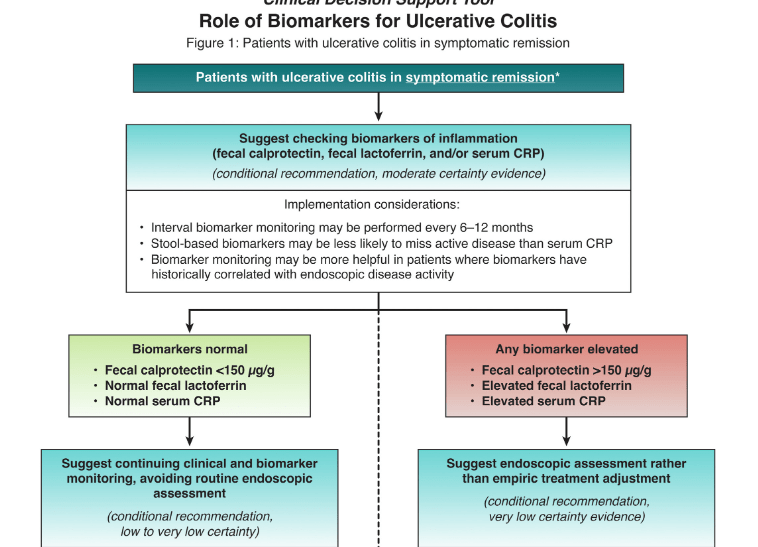
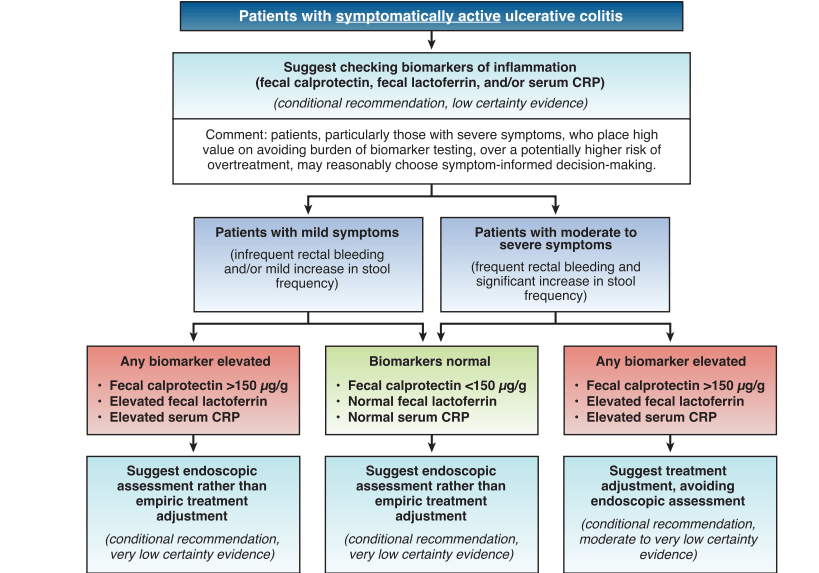
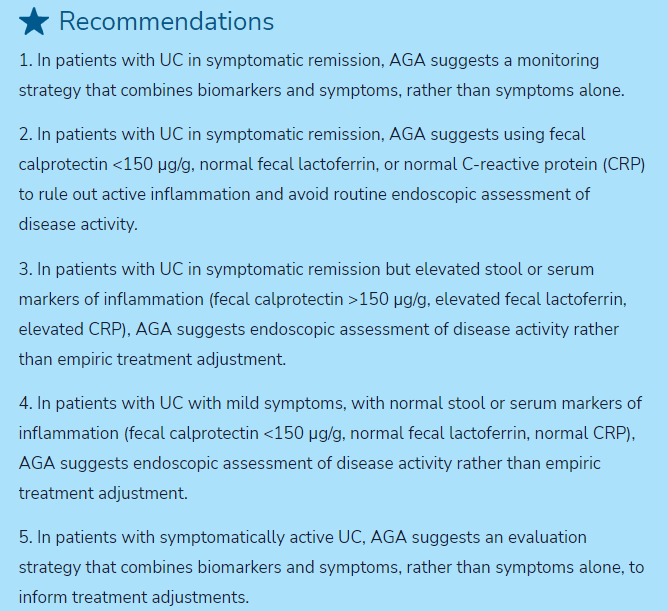

My take: By combining biomarkers with symptoms, this improves utility of more invasive testing.
Related blog posts:
- AGA Guidelines: Moderate to Severe Ulcerative Colitis
- AGA Guidelines on the Management of Mild-to-Moderate Ulcerative Colitis
- IBD Shorts: Fecal Calprotectin in UC & Medication Withdrawal, Outcome of Biosimilar Reverse Switches, Vedolizumab after Anti-TNF Therapy
- Correlating Calprotectin with Disease Severity in Pediatric IBD
- Fecal Calprotectin Monitoring Helpful at Identifying Relapse in IBD



