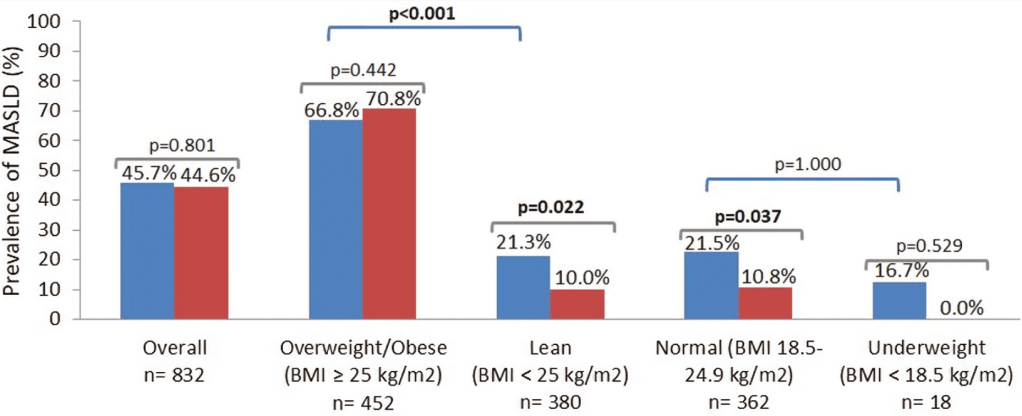
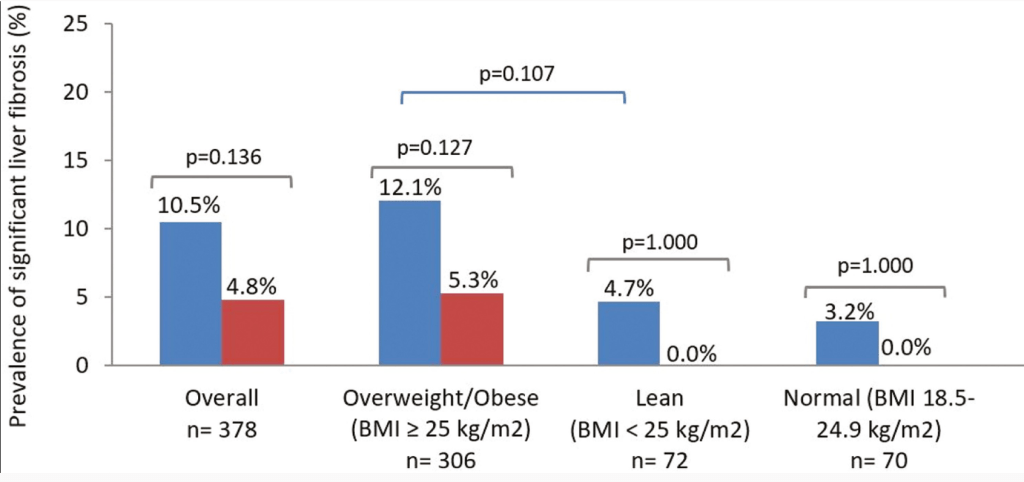
V Chen et al. Hepatology 2024; doi: 10.1097/HEP.0000000000001112. Open Access!. Resmetirom therapy for metabolic dysfunction-associated steatotic liver disease: October 2024 updates to AASLD Practice Guidance
Key points:
- Guidance recommends use of resmetirom (in adults) with F2-F3 fibrosis as determined by “imaging-based NILDAs, such as liver stiffness measurement (LSM) by vibration-controlled transient elastography (VCTE) or magnetic resonance elastography (MRE)…liver biopsy is not typically recommended for fibrosis staging in current clinical practice, [though] histologic examination remains the gold standard to quantify fibrosis.”
- “Glucagon-like peptide 1 (GLP-1) and GLP-1/glucose-dependent insulinotropic polypeptide (GIP) receptor agonists are FDA approved for the treatment of type 2 diabetes and overweight/obesity. They reduce the risk of cardiorenal complications in addition to their effects on glycemic control and weight loss.17–25 While these pharmaceutical agents are not currently approved for the treatment of MASH, phase 2 randomized, placebo-controlled clinical trials of liraglutide, semaglutide, and tirzepatide have demonstrated their efficacy in reducing steatohepatitis without worsening fibrosis and, in the case of tirzepatide, decreasing fibrosis without worsening of steatohepatitis as well.”
- “The most common treatment-emergent adverse events were diarrhea and nausea, which developed in 24% to 34% and 12% to 22% of resmetirom-treated participants, respectively…Development of hypothyroidism requiring levothyroxine replacement occurred in 1.8% of participants receiving resmetirom.”
- The authors recommend assessing response with bloodwork and noninvasive imaging at 1 yr to help determine if therapy should be continued.
My take: This article provides practical advice for using resmetirom for MASLD.
Related blog posts:
- Resmetirom (Rezdiffra) -FDA Approved for MASH with Moderate to Advanced Fibrosis
- You No Longer Have Fatty Liver Disease-You Have Steatotic Liver Disease!
- Resmetirom for MASH
- Tirzepatide for Metabolic Dysfunction–Associated Steatohepatitis (MASH) & Uptick in GLP1 Use
- Prevalence of Steatotic Liver Disease in U.S. And Risk of Complications
- Survodutide, Dual Glucagon Receptor/GLP-1 Receptor Agonist, for MASH (Phase II Trial)
- Non-Invasive Studies Often Fail to Detect Advanced Liver Fibrosis in Steatotic Liver Disease