This blog entry has abbreviated/summarized this terrific presentation; most of the material has been covered in this blog in prior entries but still this was a useful review. Though not intentional, some important material is likely to have been omitted; in addition, transcription errors are possible as well.
3rd Lecture: Prevention and management of malignancy in IBD –Dr. Thomas Ullman
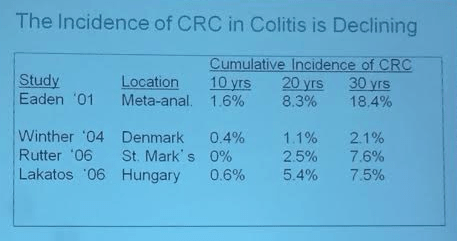
Malignancy risk (colorectal cancer [CRC]) is present with prolonged ulcerative colitis, though more recent studies have shown lower risk than in the past –not much higher than the general population.
- CRC surveillance–colonoscopy monitoring after 8-10 years. Typically colonoscopy every other year for most patients, every year in higher risk patients (eg. PSC).
- Unclear if chemoprevention is effective (5-ASA, thiopurines, others).
- Chromoendoscopy “has not been consensus on its use in our field (yet).” It is time consuming and expensive and unclear if it will improve outcome.
Does medical therapy for IBD predispose to developing cancer?
- Thiopurines increase the risk of malignancy. (Pasternak et al) though the risk returns to near baseline when stopped according to study below.
- No overall increased risk with anti-TNF agents with RCTs (may not follow patients long enough) but also not seen in Danish registry either (JAMA study)
- Lymphoma risks: age, immunodeficiency, EBV
- EBV negative are at risk for HLH with thiopurines
- HTSCL ~200, >90% men and >90% <35 years. NOT EBV-related. Has not been identified in anti-TNF monotherapy.
- Skin cancer –main concern is in non-melanoma skin cancer (possibly melanoma too). Skin cancer increase has not been noted with methotrexate. Prevention: Skin care, and annual dermatology visits.
- Cervical cancer—likely increased risk in IBD, probably due to thiopurine exposure and reduced immune surveillance. Prevention: HPV vaccination, Pap testing.
- Urinary Tract cancers –especially in those >65 years with thiopurine exposure