From AGA on YouTube: Twistomy (~1 min)

Twisting of the external ring allows control of ostomy flow and the use of intermittent drainage rather than always relying on an ostomy bag.
More information at product website: Twistomy

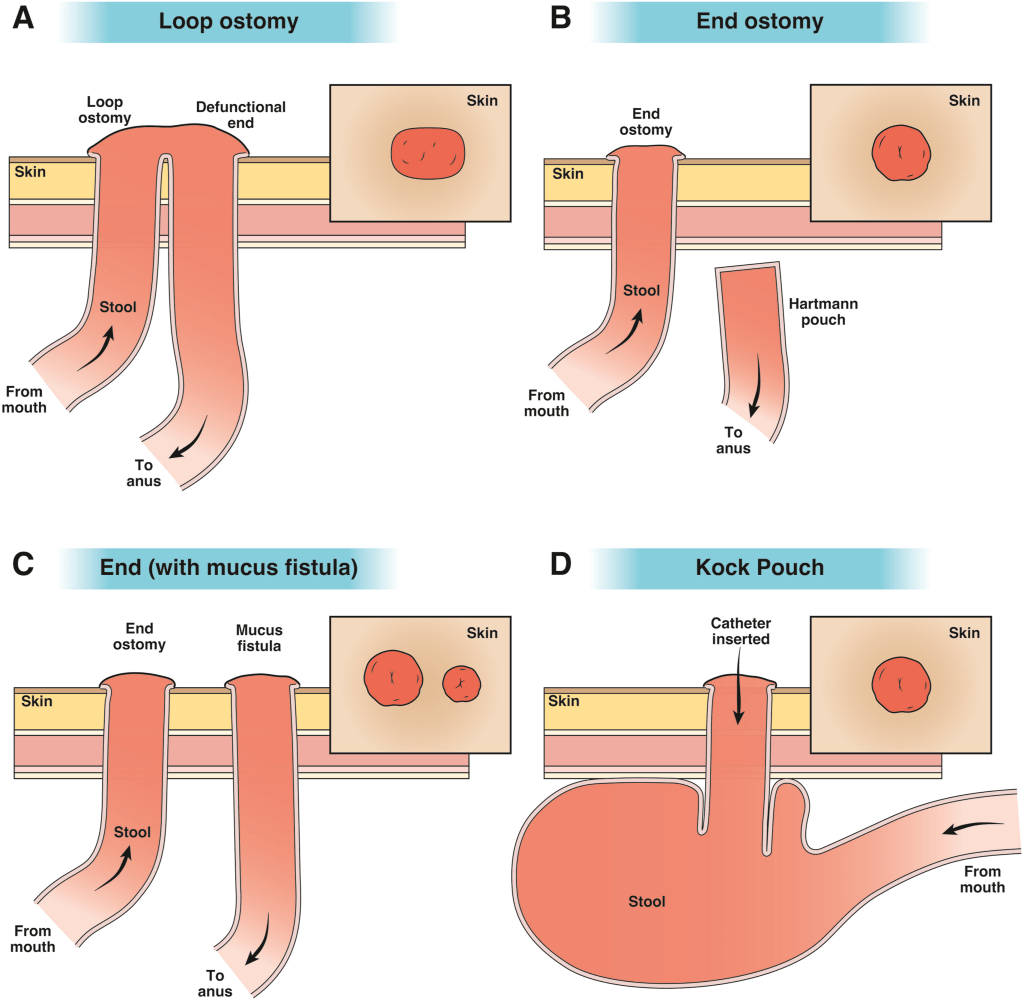
K Mullin, RM Rentea, M Appleby, PT Reeves. Pediatrics in Review 2024; 45: 210-224. Gastrointestinal Ostomies in Children: A Primer for the Pediatrician
Like yesterday’s article on GTs, this is another terrific review with plenty of helpful images and advice regarding ostomy management.



My take: This is a very useful resource. Even a quick read will make clinicians appreciative of having the assistance wound ostomy nurses.
Related blog posts:
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.
TL Hedrick et al. Clin Gastroenterol Hepatol 2023; 21: 2473-2477. Open Access! AGA Clinical Practice Update on Management of Ostomies: Commentary
This article is a helpful review on ostomy care. The article reviews approaches to common problems including early high ostomy output, ostomy leakage, stoma retraction, mucocutaneous separation, dermatological problems, chronic high ostomy output, parastomal hernia, and stoma prolapse. A few of their comments:
Related blog posts:
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.
A recent article ( David JG, Jofriet A, Seid M, et al. “A Guide to Gutsy Living”: Patient-Driven Development of a Pediatric Ostomy Toolkit. Pediatrics. 2018;141(5): e20172789) describes “A Guide to Gutsy Living”: Patient-Driven Development of a Pediatric Ostomy Toolkit (Full Text)
From ImproveCareNow: Download a free copy of the Ostomy Toolkit
Background:
The education we received about our ostomy surgery was brief and focused only on basic skills regarding caring for an ostomy, including changing and emptying the bag, but did not address concerns we had about living with ostomies as part of our everyday lives. This educational void placed the burden on us as patients to find resources on our own, decide if the information was appropriate, and determine if it was reliable and accurate.
In this article, we describe how we, as patients, harnessed the capacity of a collaborative chronic care network1 and were supported to develop a resource that patients needed.
Methods:
We started a national task force of interested patients and parents who had experiences with ostomies to develop a pediatric ostomy toolkit. The task force was composed entirely of patients and parents and consisted of 7 patients and parents
After a literature review, we asked task force members to identify questions and topics related to living with an ostomy, including questions members had preoperatively, immediately postoperatively, and in the extended time since their surgeries. From this prompt, our group generated a list of topics all patients and parents agreed on based on the shared concerns, insights, or questions our task force members had around ostomy surgery… After the creation of the toolkit, we reached out to clinicians to provide clinical review.
Results:
Our final 19-page, colorful toolkit included topics relating to friends, school, travel, ostomy supplies, clothing, playing sports, using humor to cope, emergency kits, educational issues (eg, 504 plans), “Gastronauts” (Gastronauts are freely available puppets with ostomies), and ostomy medical language…The pediatric ostomy toolkit was posted on the ICN Exchange platform
My take (borrowed from authors): In our patient- and parent-led toolkit project, we demonstrate how patients and families can self-organize and ask clinicians to consult to create needed resources within a network
Resources:
MI Abdalla et al. Inflamm Bowel Dis 2016; 22: 2658-64. This article reviewed the impact of an ostomy on QOL (quality of life) for Crohn’s disease patients. n=402 with ostomy compared with 4331 CD patients without.
Key findings:
WKM Liew et al. J Pediatr 2016; 178: 227-32. In this study with 16 patients (aged 6-24 years) who received thalidomide, more information on neuropathy is provided. “All subjects with cumulative doses greater than 60 g developed polyneuropathy.” 4 of 5 subjects receiving the drug for >20 months developed neuropathy. Two important points:
V Collij et al. Inflamm Bowel Dis; 2016; 22: 2562-70. “We identified drugs that target the proteins encoded by IBD candidate genes.” Key finding: There were 113 drugs that could potentially be used in IBD treatment, including 14 known IBD drugs, 48 drugs that are/have been tested for IBD, 19 being tested for other inflammatory diseases, and 32 new investigational medications.
Recently, I received a post from Oley Foundation (Linda May) asking me whether I was going to its convention. While I am not, I did want to share that link:
http://www.oley.org/annualconf.html
The conference is in lovely Redono Beach, CA, right on the beach. We have miles of running paths, beautiful beaches, on site tennis courts, and swimming pool . To quote other MDs, “the Oley Annual conference is the most important clinical conference I attend all year…”
Also, Oley website is a good link for patients with enteral tubes, ostomies, and central lines. http://oley.org/
Many questions and how-to advice available. For example, look at this link if interested in advice about swimming with central line, or enteral tube: http://www.oley.org/Swimming.html