V Volkert et al. JPGN Reports. 2025;1–7. Long-term outcomes of intensive multidisciplinary intervention for feeding tube dependence and chronic food refusal
Methods: The researchers conducted a 17‐item Qualtrics survey of patients who participated in intensive multidisciplinary intervention treatment to improve the volume and variety of solid food intake and replace enteral feeding due to chronic food refusal an average of 6 years following intervention. 75 met eligibility criteria; 36 caregivers (48%) completed the survey
Key findings:
- Most patients (80%) who achieved full wean from feeding tube dependence at program discharge maintained their wean at the time of the survey
- Most caregivers (89%) described their child’s relationship with food as “good” or “neutral”
My take:
- Our group works closely with the authors and appreciate all of their help
- Survey studies have a lot of limitations and often conclusions are hampered by low participation
- It looks like intensive feeding therapy has good durability. It would be interesting if we could know what would have happened to these children without therapy. How many would have gradually improved on their own?
Related blog posts:
- Good Luck Getting Intensive Feeding Therapy
- Highly Prevalent Pediatric Feeding Disorders
- Expanding Feeding Programs for Children with Autism
- Dr. Praveen Goday: Tips on Managing Feeding Problems (Part 1)
- Dr. Praveen Goday: Tips on Managing Feeding Problems (Part 2)
- Feeding Aversions –A Personal Journey
- Nutrition Week (Day 3) Multidisciplinary Feeding Disorders
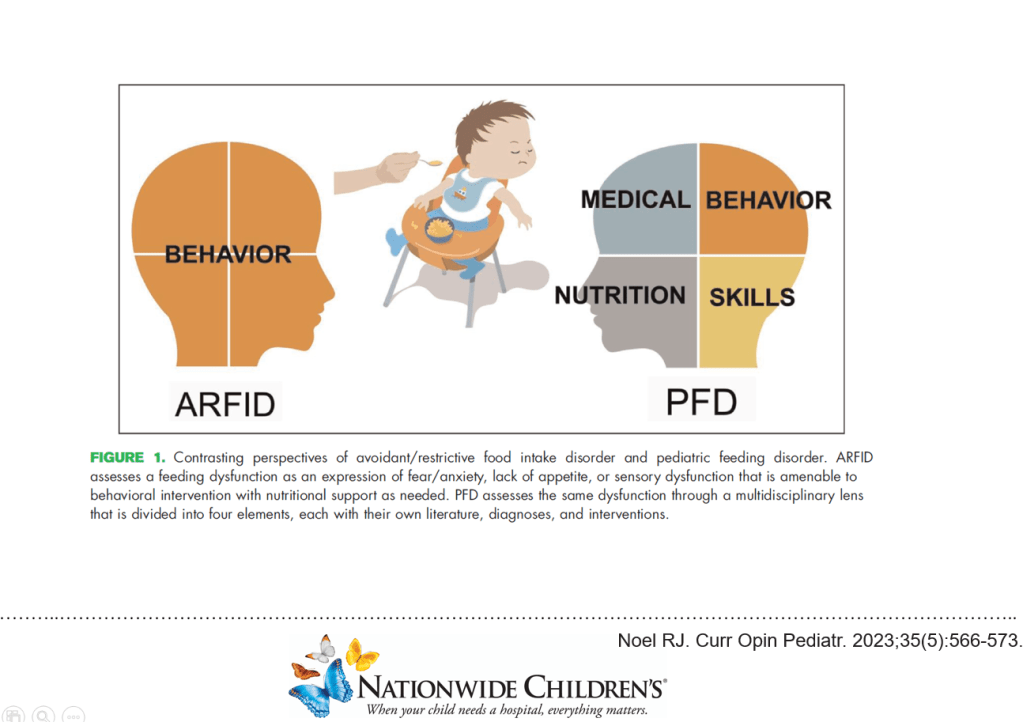
- Prevalence of Avoidant/Restrictive Food Intake Disorders in Pediatric Neurogastroenterology