K Takenaka et al. Clin Gastroenterol Hepatol 2025; 23: 1991-2000. Open Access! Inadequate Efficacy of Biologics for Treating Proximal Ileal Lesions in Crohn’s Disease: A Prospective Multicenter Study
This multicenter prospective study (n=253) examined efficacy of treatment in patients with proximal ileal disease using balloon-assisted enteroscopy (BAE). The recruited patients had a mean disease duration of 4 years. 52% were naive to biologic treatment at baseline.
Key findings:
- At baseline, 74 patients (29.2%) had proximal ileal ulcerations without terminal ileal ulcerations
- At week 26, after treatment with anti-TNF therapy (n=103), ustekinumab (n=99) or vedolizumab (n=51), endoscopic remission was achieved in 91 patients (36.0%). Of the patients with complete ulcer healing of the terminal ileum, 28.6% (22/77) had residual ulcers in the proximal ileum
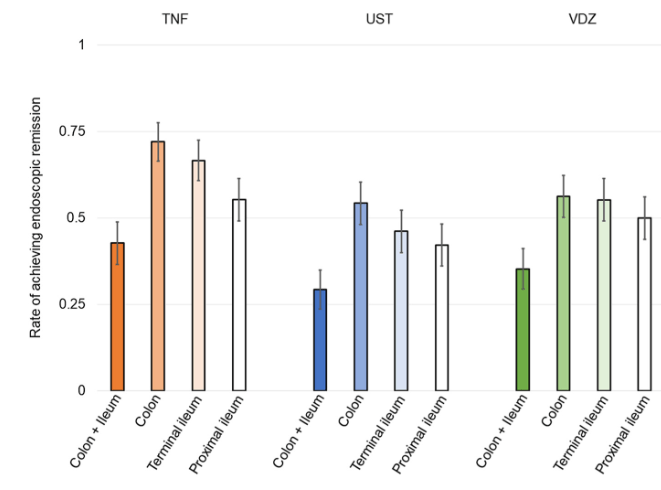
- The rate of endoscopic remission in the proximal ileum (50.9%) was relatively lower compared with the colon (63.4%) and terminal ileum (56.7%)
- After a median follow-up of 134 weeks, residual ulcerations in the proximal ileum were associated with a poorer prognosis (P = .0126 for hospitalization and P = .0014 for surgery). In contrast, there was no significant differences in hospitalization and surgery associated with endoscopic activity vs remission in the colon or terminal ileum.
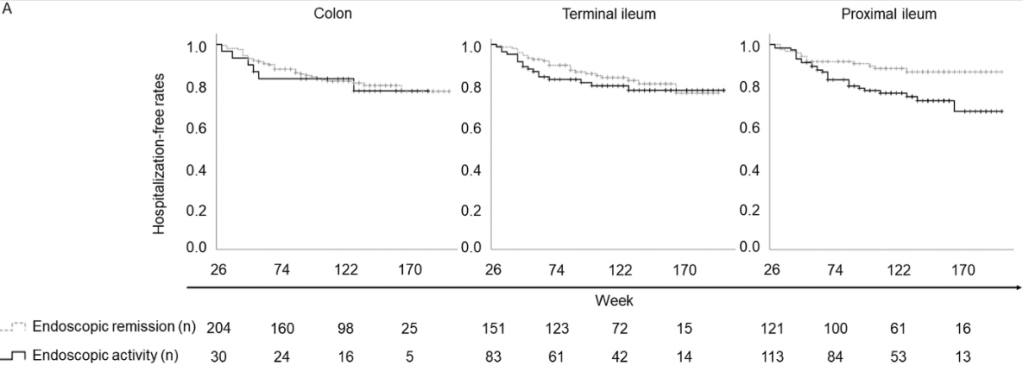
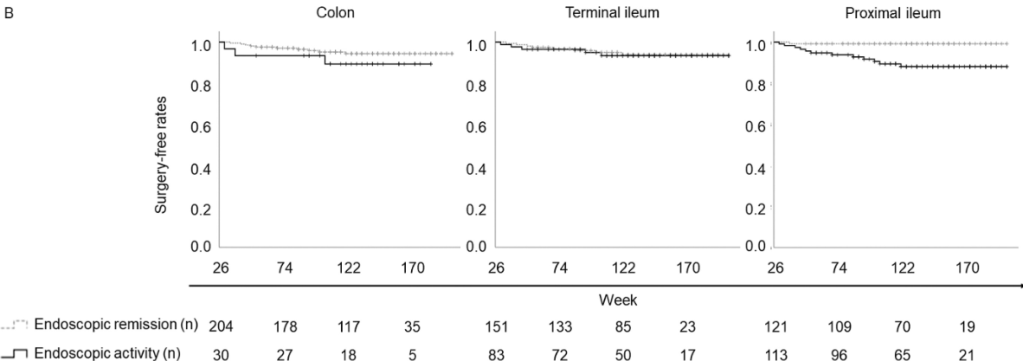
Discussion: Residual “proximal ileal ulcerations … are associated with a poorer prognosis…Additionally, we confirmed that proximal ileal inflammation is less responsive to biologic therapies compared with colonic inflammation. Although the reasons for this disparity remain unclear”
My take: Balloon-assisted enteroscopy is not frequently used in the setting of inflammatory bowel disease, particularly in pediatrics. MRE is typically used to follow proximal small bowel disease, though it has less sensitivity for luminal mucosal disease.
Related blog posts:
- Which Crohn’s Disease Ulcerations Are Harder to Treat — Small Bowel or Colon?
- Toronto Consensus Guidelines for Luminal Crohn’s Disease
- Transmural Disease, Biomarkers, and Correlation between MRI and Endoscopy
- Calprotectin Less Accurate for Isolated Ileal Crohn’s Disease
- Expert Guidance on Inflammatory Bowel Disease (Part 3) | gutsandgrowth