Recently, Ben Gold handed me a supplement which alluded to the case of “the blind men and the elephant.” So, of course, I wanted to know more about this.
According to Wikipedia:
In various versions of the tale, a group of blind men (or men in the dark) touch an elephant to learn what it is like. Each one feels a different part, but only one part, such as the side or the tusk. They then compare notes and learn that they are in complete disagreement. The stories differ primarily in how the elephant’s body parts are described, how violent the conflict becomes and how (or if) the conflict among the men and their perspectives is resolved. In some versions, they stop talking, start listening and collaborate to “see” the full elephant. When a sighted man walks by and sees the entire elephant all at once, the blind men also learn they are all blind. While one’s subjective experience is true, it may not be the totality of truth. If the sighted man were deaf, he would not hear the elephant bellow.
It has been used to illustrate a range of truths and fallacies; broadly, the parable implies that one’s subjective experience can be true, but that such experience is inherently limited by its failure to account for other truths or a totality of truth. At various times the parable has provided insight into the relativism, opaqueness or inexpressible nature of truth, the behavior of experts in fields where there is a deficit or inaccessibility of information, the need for communication, and respect for different perspectives.
The rest of the supplement regarding chronic health consequences following acute enteric infections was less interesting but probably more important than learning a new anecdote.
The introduction notes that nearly 600,000 children under 5 years die from dehydrating diarrhea each year. Many more suffer from consequences of disease-associated malnutrition with both physical and cognitive deficits.
Articles in supplement:
- Am J Gastroenterol Suppl 2016; 3: 4-11. –details diarrhea-associated years lived with disability 51 per 100,000 in developed regions compared with 685 in developing regions.
- Am J Gastroenterol Suppl 2016; 3: 12-23. –details the likelihood of consequences following enteric infections, including functional GI disorders, inflammatory bowel disease, celiac disease (data limited), Guillain-Barré syndrome, hemolytic uremic syndrome, chronic fatigue, and neurologic sequelae.
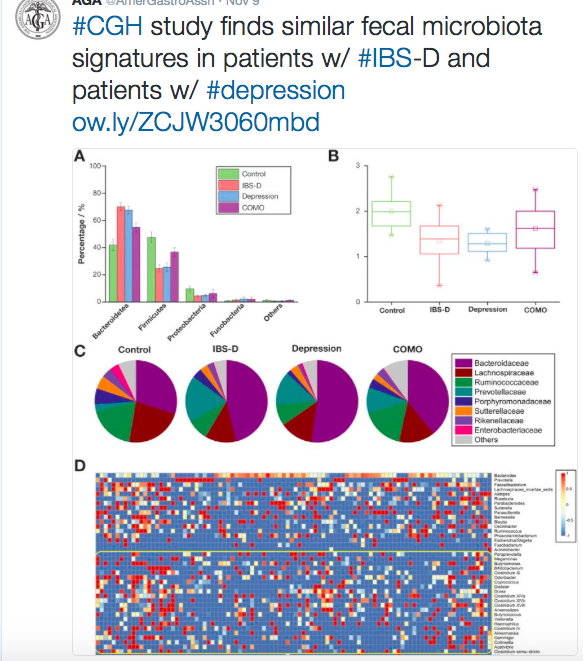
- Other articles in the supplement describe changes in the microbiome, the micorbiome-gut-brain axis, and the relationship between autoimmunity and irritable bowel.