This blog entry has abbreviated/summarized the presentations. Though not intentional, some important material is likely to have been omitted; in addition, transcription errors are possible as well. All of the speakers had terrific presentations. The course syllabus is attached:
PG Course Syllabus 2014
The 3rd Module had a “potpourri” of GI problems.
Extraesophageal Manifestations of Gastroesophageal Reflux –Ben Gold, MD (GI Care For Kids, Atlanta) (pg 86)
“Is reflux really the scurge of the earth and the cause of every malady known to human-kind in the head, neck, and lungs…?“
Key points:
Airway protection: “Aerodigestive disease reflexes are intact by 38 weeks gestation.”
Central deglutition apnea: a normal protective mechanism to prevent aspiration during swallowing. (Hasenstab KA, Jadcherla, S. J Pediatr 2014; 165:250-255). No proof at present that central apnea is caused by reflux though there is a biologic plausibility.
“Although reflux causes physiologic apnea, it causes pathologic apneic episodes in only a very small number of newborns and infants.” “When reflux causes pathological apnea, the infant is more likely to be awake and the apnea is more likely to be obstructive in nature.”
Laryngeal Reflux:
- Chronic cough, chronic laryngitis, hoarseness, and asthma may be associated with GERD BUT the data showing a relation between reflux and upper airway disease are weak
- Airway symptoms attributed to reflux in adults include hoarseness, chronic cough, and globus sensation
- Affected adults rarely have typical reflux symptoms
- The sensitivity of laryngoscopic findings to identify reflux disease are poor. Sherman et al. Am J Gastroenterol. 2009;104:1278-95. Vandenplas et al. J Pediatr Gastroenter Nutr. 2009;49:498-547.
Asthma:
“Chronic cough, chronic laryngitis, hoarseness and asthma are multifactorial disease processes and acid reflux can be an aggravating cofactor.” GER is an unlikely contributor to asthma if reflux testing is negative.
“Two NIH-funded blinded, randomized placebo-controlled trials (RCT), one in adults (using esomeprazole), one in children (using lansoprazole) showed NO difference in asthma outcomes comparing placebo and acid suppression therapy”
Multi-Channel Intraluminal Impedance/pH probe studies: Pediatric studies are critically needed to determine if knowing the amount of nonacid reflux changes treatment or outcome
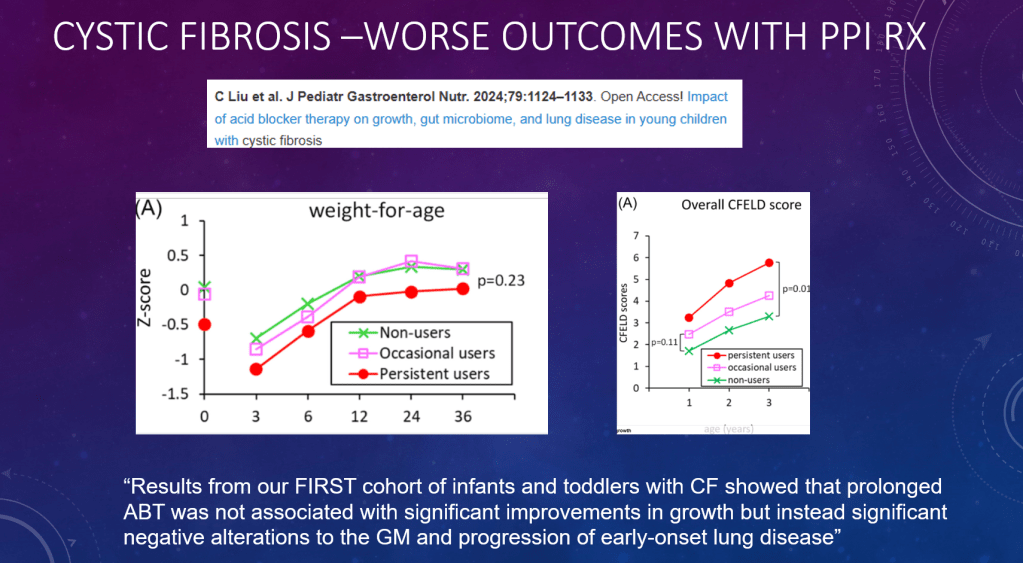
Proton Pump Inhibitors can cause gastric bacterial overgrowth (Rosen R et al JAMA Pediatr 2014; JAMA Pediatr. doi:10.1001/jamapediatrics.2014.696)

Ben Gold (speaker) and Jay Hochman prior to 5K Run
Related blog posts:
EoE: PPI, PPI-REE, TCS, OVB, SFED, 4FED….…Alphabet Distress — Sandeep K Gupta, MD (Indiana University) pg 105 in Syllabus
Treatment endpoints discussed -histologic, symptomatic, fibrosis, etc.
- Proton pump inhibitor responsive eosinophilic esophagitis (PPI-REE) may work by blocking STAT6 binding to Eotaxin-3 promoter rather than by acid suppression (PLos ONE 2012;7:e50037). PPIs work (eos <6/hpf) in in 30-40%. May need high dose to work long-term (Dr Molina-Infante – DDW 2014)
- Topical corticosteroids (TCS) -higher dose = better response. (Budesonide. Gupta SK, Vitanza J, Collins, MH Clin Gastro Hepatol 2014 [ePub], Fluticasone. Butz BK. Gastroenterology 2014). Clinical symptoms do not correlate with histologic response. Discussed long term safety concerns.
- Reviewed diets -elemental, targeted, 4-food elimination and 6-food elimination.
Related blog posts:
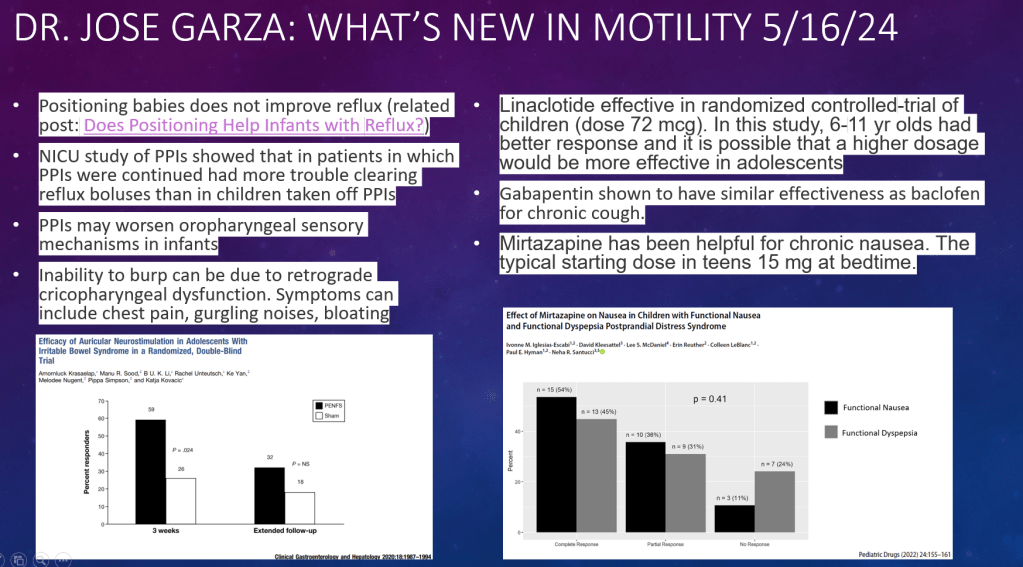
“Gotta keep on movin”: New tricks and treatments for motility disorders –Carlo DiLorenzo (Nationwide Children’s Hospital) pg 116 in Syllabus
Key points:
- Most important motility study is a normal study. If normal study, then there is more concern for sensory dysfunction. Look for significant findings on motility studies not minor changes.
- Key to confirm if motility disorder is present. Hx/o small intestinal transplant in medical child abuse/Munchausen syndrome by proxy (Trans Proc 1996; 28: 2790)
- New tool: wireless motility capsule (J Pediatr. 2013;162:1181-7)
- Easier to obtain full thickness biopsies (Gastrointest Endosc 2011;73:949-54)
Treatments reviewed -“try everything”
- prucalopride (JPGN 2014; 57: 197-203
- cisapride -still available
- lubiprostone (JPGN 2014;58:283–291)
- linaclotide boxed warning not for <17 years of age –though has been used by motility specialists
- cyproheptadine (J Pediatr 2013; 163: 261-7) –use in dyspepsia
- fludrocortisone -used in orthostatic intolerance
- augmentin -for small bowel motility (JPGN 2012;54: 780–784)
- octreotide -for bowel motility
- pyridostigmine (Colorectal Disease 2010 12, 540–548)
- iberogast
- botulinum toxin (Gastrointest Endosc. 2012 ;75:302-9)
- treat bacterial overgrowth
- surgery: Jube, GJ tube, ileostomy. “Every child with pseudoobstruction on TPN needs a gastrostomy and an ileostomy –(me, now)”
- gastric electrical stimulation
- emerging treatment: Elobixibat (for constipation) Expert Opin. Investig. Drugs
Related blog posts:
What’s New in the Diagnosis and Management of Constipation –Manu Sood (Children’s Hospital of Wisconsin) -page 130 in Syllabus
Reviewed recent guidelines from NASPGHAN
“Miralax is considered a 1st line agent”
Outcomes in children with constipation:
- Almost 50% of patients experienced at least one relapse in first 5 yrs.
- Almost 20% of children were symptomatic at 10 yrs. follow up (Bongers ME, et al. Pediatrics. 2010)
Pointers:
- Slow transit is common
- Rectal compliance does not predict success with treatment. Van den Berg MM, et al. Gastroenterology 2009. Patients with mega-rectum may have motility disturbance as well.
- Success rates for antegrade continence enemas (ACE) 65% to 89%. Colon manometry can help predict ACE success. Up to 40% may be able to stop ACE w/in 2 years
Related blog posts: