1st Study: M Lamba et al. Clin Gastroenterol Hepatol 2021; 19: 573-579. Full text: Trends in Incidence of Autoimmune Liver Diseases and Increasing Incidence of Autoimmune Hepatitis
This was a population-based prospective study from Canterbury, New Zealand
Key findings:
- Overall incidence rates were 1.93 per 100,000 for AIH (95% CI, 1.58–2.34), 0.51 per 100,000 for PBC (95% CI, 0.33–0.73), and 0.92 per 100,000 for PSC (95% CI, 0.68–1.21).
- The incidence rate of AIH was significantly higher during the period of 2014–2016 (2.39 per 100,000; 95% CI, 1.76–3.23) than during the period of 2008–2010 (1.37 per 100,000; 95% CI, 0.91– 2.06) (P < .05). Incidences of PBC and PSC did not change significantly.
- In 2016, prevalence values were 27.4 per 100,000 for AIH (95% CI, 23.58–32.0), 9.33 per 100,000 for PBC (95% CI, 7.13–12.05), and 13.17 per 100,000 for PSC (95% CI, 10.56–16.42).
My take: This study indicates that autoimmune hepatitis has been increasing in incidence.
Related blog posts:
- Predicting Outcomes in Childhood Autoimmune Hepatitis
- Autoimmune Hepatitis -Early Response Associated with Remission
- Online Aspen Webinar -Autoimmune Hepatitis
- Using Less Steroids for AIH
2ndStudy: ZM Younossi et al. Clin Gastroenterol Hepatol 2021; 19: 580-589. Full text: Nonalcoholic Steatohepatitis Is the Most Rapidly Increasing Indication for Liver Transplantation in the United States
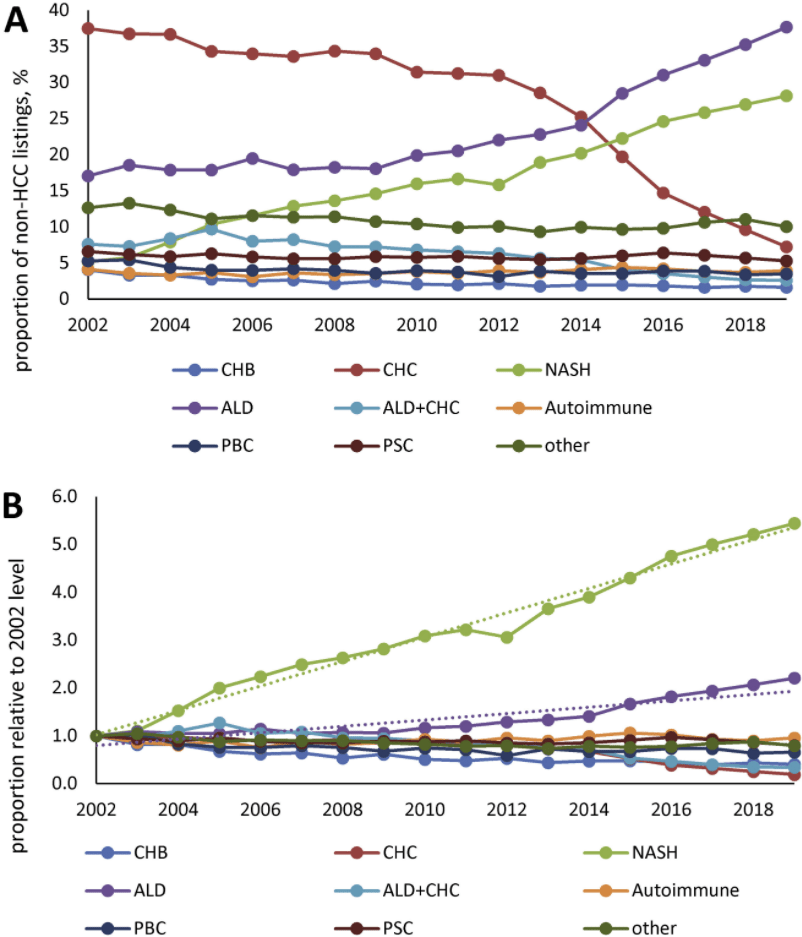
This study was an analysis of data from the Scientific Registry of Transplant Recipients (2002 through 2019).
Key findings:
- In 2002, the most common etiologies of non-acute liver failure on the liver transplant waitlist (in patients without HCC)
- In 2019, among patients without HCC, NASH was the second leading indication for liver transplantation (28% of patients), after ALD (38% of patients). were chronic HCV infection (37%) and ALD (16%), whereas only 5% had NASH
- HCC accounted for 27,799 patients (16.5%) and was commonly due to chronic HCV throughout study period
My take: Demand for liver transplantation has NOT improved despite curative therapy for chronic hepatitis C. This is due to increased liver failure related to fatty liver disease and alcoholic liver disease.
Related blog posts:
- Bad Fatty Liver Disease Can Get Worse Quickly
- Liver Shorts April 2019 Obesity/NAFLD and alcoholic liver disease are driving an increase in HCC and liver cancer mortality
- Alcohol #1 reason for liver transplantation
- Alcohol in the setting of fatty liver disease