JM Perrin, TL Cheng. NEJM 2025; 393: 1869-1872. “Truly Prioritizing Child Health — The Missed Opportunities of the MAHA Commission”
This commentary welcomes the attention to child health which was a focus of the MAHA commission. This review provides perspectives on the stated policy aims and on what else is needed.
An excerpt:
The [MAHA] commission has highlighted four specific areas of concern: poor diet, environmental chemicals, lack of physical activity and chronic stress, and overmedicalization. The strategy outlined in the MAHA Commission’s recent report, however, misses real opportunities to address the chronic disease epidemic and “whole-person health”…
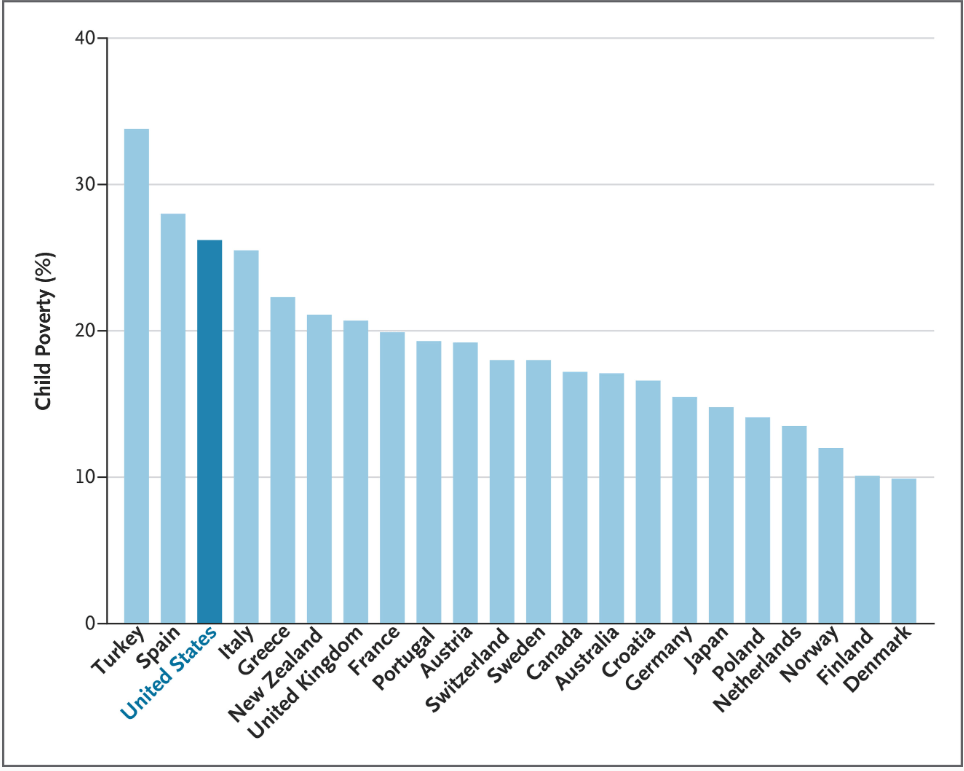
The MAHA Commission’s view of the state of U.S. child health ignores leading contributors to rising childhood morbidity and mortality: firearm injuries (the leading cause of death among U.S. children), drug overdoses, and motor vehicle injuries. Most striking is the commission report’s silence regarding the association of poverty with poor child health… which contributes to higher rates of asthma, obesity, and mental health conditions...
The first MAHA priority, children’s diets, has long been a concern of the U.S. child health community, particularly the intake of sugar-sweetened beverages, excessive portion sizes, and food additives. But pediatricians and researchers also know that food insecurity, food-industry marketing practices, and limited access to healthy foods are prime drivers of childhood obesity rates. Nutritious meals require money…
The MAHA strategy recommends marginal changes to the diets of U.S. children, such as reducing the use of food dyes and reducing consumption of ultraprocessed foods, even as the government is increasingly limiting public food assistance.
The commission’s focus on environmental chemicals is appropriate, given that exposures to potentially toxic chemicals in foods, household supplies, cleaning agents, farm supplies, and elsewhere have grown dramatically. The MAHA strategy provides little relief, however: a few research projects and no regulatory change…The MAHA report stops short of recommending the research and regulatory reform necessary for identifying, restricting, and mitigating harmful exposures.
Concerns about physical activity and stress are also justified. Many studies have documented alarming declines in physical activity, examined the causes and effects, and found associations with mental health and well-being… Strengthening early-childhood, school-based, and community-based physical activity programs, as well as social media strategies for promoting lifestyle changes, could improve health and reduce stress among young people, but the MAHA Commission mainly orders schools and communities to increase physical activity.
Finally, the commission has raised concerns about medications, especially stimulants and psychotropic agents…In response, the MAHA Commission primarily proposes studying prescribing patterns and “solutions that can be scaled up to improve mental health.” It does not address more fundamental ways of changing medication use…
Despite its attention to children’s health, the MAHA Commission’s lengthy list of aspirations and recommended changes is unlikely to make a real impact. Instead, next steps should include implementing policies, programs, and research supported by the strong evidence base that clinicians and investigators have built painstakingly for many years.
My take: The policies pursued by the current administration like limiting food dyes do not target the big drivers of poor health outcomes in children.
The authors of this commentary also “chaired the National Academies of Sciences, Engineering, and Medicine (NASEM) study described in “Launching Lifelong Health by Improving Health Care for Children, Youth, and Families”1 [which] provides clear, evidence-based lessons that could help in achieving MAHA objectives.”
Reference: National Academies of Sciences, Engineering, and Medicine. Launching lifelong health by improving health care for children, youth, and families. Washington, DC: National Academies Press, 2024 (https://nap.nationalacademies.org/catalog/27835/launching-lifelong-health-by-improving-health-care-for-children-youth-and-families).
Related blog posts:
- “How to Make America Healthy: the Real Problems — and Best Fixes”
- Longevity Gap Present Even in Wealthy Americans
- Ten Americas: Examining Health Disparities and Life Expectancy
- “Proposed Medicaid Cuts Could Lead to Thousands of Preventable Deaths Annually” & Personal Message
- How Putting America First is Undermining Health Outcomes Here and Globally
- No Exaggeration: Too Many Children Are Dying in the U.S.
- Firearms: #1 Cause of Pediatric Deaths & Households with Guns =More Deaths