A useful review (Clin Gastroenterol Hepatol 2013; 11: 6-12) provides information on these clinical problems.
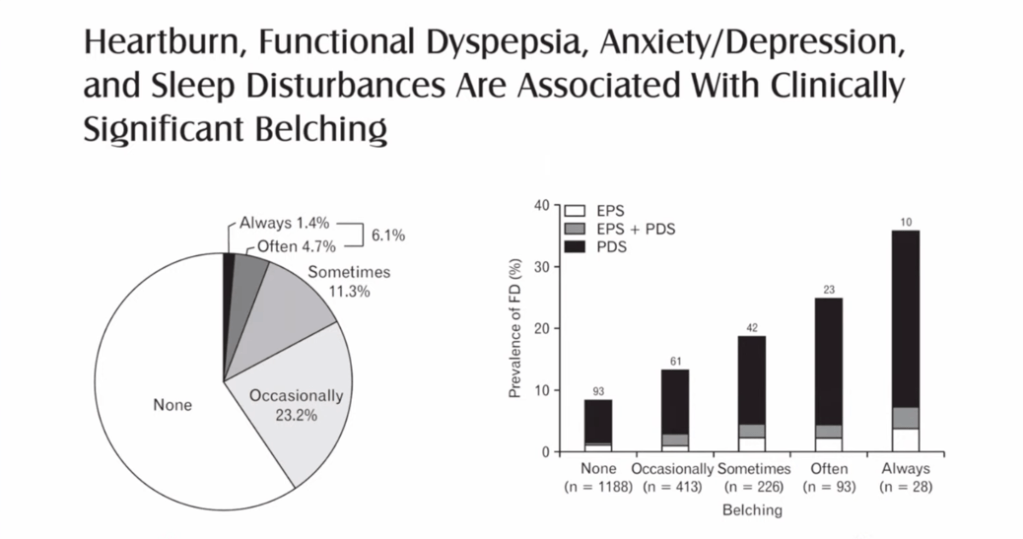
Belching or eructation can be divided into gastric belches which are normal and supragastric belching. Supragastric belching which is a behavior (not a reflex), is often provoked by stress. Air does not originate from the stomach or air swallowing (aerophagia). The most common mechanism: a contraction of the diaphragm causes negative pressure in the chest and allows air to be suctioned into the esophagus. It is expelled subsequently as a belch. In some instances, it can occur up to 20 times a minute. Supragastric belching does not occur during sleep and usually does not occur during speaking.
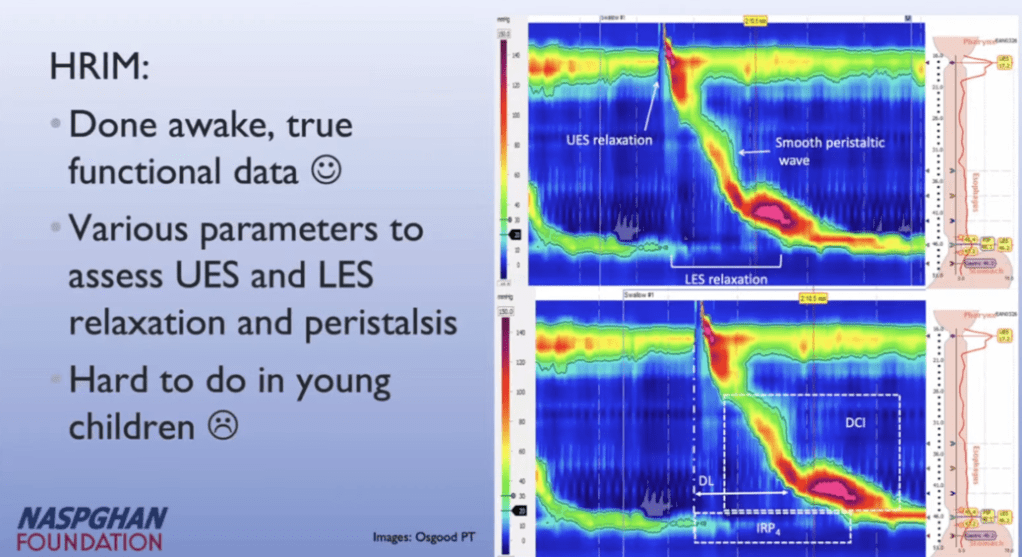
A clinical diagnosis usually is sufficient, though esophageal impedance can document these events as well.
Management:
- Explain physiology to patient
- Consider psychiatric evaluation when appropriate
- Glottis training by qualified speech therapist –needs to be aware of mechanism (that belching is not due to aerophagia).
- Alternative treatment could include cognitive behavior therapy, baclofen, hypnosis or biofeedback
Hiccups (singultus) are abnormal if lasting more than 48 hours.
Hiccups (at least in adults) have more likelihood of underlying pathology than belching. This review suggests workup including blood tests (CBC, CMP, Amylase/lipase, CRP, Cortisol) and consideration of EKG, CT of chest, Upper endoscopy, MRI of brainstem, and esophageal impedance.
Physical maneuvers have usually been tried and include the following: scaring the patient, rapid drinking, eyeball compression, holding breath, biting a lemon, swallowing sugar, and sniffing vinegar. A good differential diagnosis is given as well in this review -though many cases are idiopathic.
In the U.S. the only approved drug treatment is chlorpromazine. Typical starting dose for adults with this condition is 25 mg 3-4/day. Potential side effects include drowsiness and rarely tardive dyskinesia. Potential alternatives include baclofen and gabapentin. Numerous other agents and even surgical options are listed in this review that have been reported in case studies.
Aerophagia indicates excessive swallowing of air (capable of inducing symptoms like bloating or pain). No controlled studies have been completed. Expert opinion suggests using a nasogastric tube and sedatives like lorazepam in severe acute cases. In more typical chronic cases, advice includes restriction of carbonated beverages and possibly speech therapy. Agents like simethicone may be helpful. Laxatives may be helpful in some cases as well.
Related posts:
Treatment for rumination and belching | gutsandgrowth