Recently Dr. Squires gave our group a terrific lecture. I have taken some notes and shared some slides. There may be inadvertent omissions and mistakes in my notes.
Key points:
- 2023 AASLD Practice Guidance is very helpful and Dr. Squires considers its advice akin to a ‘North Star’

- There are several etiologies for the sclerosing cholangitis phenotype – including primary disorders and secondary causes.


- Pancolitis is most common presentation of IBD with PSC, often with rectal sparing and backwash ileitis

- PSC often has subclinical inflammation and poor growth. PUCAI scores typically underestimate IBD activity

- Diagnosis can be challenging – but often “I know it when I see it”



- MMP-7 is still being studied as a biomarker. Thus far, it appears a little better than GGT and Alk phos as a marker for biliary injury
- ERCP should be avoided as part of diagnostic workup but is important for therapeutic intervention

Deneau et al (Hepatology 2017; 66: 518) study wit 781 children has a wealth of information on natural history. In children, 38% developed portal HTN and 25% developed biliary complications over 10 years. However, once these complications developed, the need for transplantation develops more quickly. Median survival with native liver after the development of portal HTN was 2.8 yrs and it was 3.5 yrs after development of biliary strictures



- Cholangiocarcinoma is rare in pediatrics ~1%
- ASC (overlap of AIH and PSC) is fairly common in children and often a manifestation of early PSC. Many evolve to PSC without overlap features. Dr. Squires counsels families that most patients will need multiple biopsies to help determine need for ongoing immunosuppression

- In patients with IBD, some liver test abnormalities and autoimmune features may be transient. Some watchful waiting may be beneficial prior to extensive evaluation
- Multiple factors can predispose to PSC, including EBV infection which is associated with OR 12. Genetics, environment, immune dysregulation, toxic bile acids, microbiome, leaky gut/inflammation are additional factors
- SCOPE is very useful prognostic tool


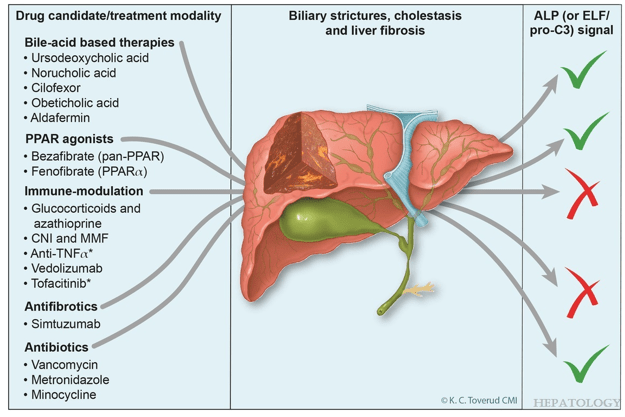
- Ursodeoxycholic acid (UDCA) is a first line therapy. However, if no response to treatment, it is likely not beneficial



- Oral vancomycin has not been proven to improve liver outcomes in PSC thus far (not recommended by AASLD 2023 Practice Guidance). However, further studies are ongoing and it has been associated with improvement in IBD activity




Related blog posts:
- ESPGHAN Guidelines for PSC in Children (2025)
- AASLD 2023 Practice Guidance for Primary Sclerosing Cholangitis and Cholangiocarcinoma
- Liver Transplantation for PSC: Long-term Outcomes and Complications
- Development of Primary Sclerosing Cholangitis in Pediatric Patients with Inflammatory Bowel Disease
- PSC in IBD
- How Primary Sclerosing Cholangitis Alters Outcomes in Inflammatory Bowel Disease | gutsandgrowth
- Cholangiocarcinoma Risk in Pediatric PSC-IBD Plus one
- Aspen Webinar 2021 Part 5 -Autoimmune Liver Disease & PSC | gutsandgrowth
- Online Aspen Webinar (Part 3) -Primary Sclerosing Cholangitis
- Big Study of Primary Sclerosing Cholangitis -Pediatrics 2017
- Active Colitis More Likely in Children in Clinical Remission Who Have PSC and IBD
- Easy Advice for Pediatric Hepatologists: PSC Guidelines from AGA Best practice advice 6: “Surveillance for cholangiocarcinoma should not be performed in PSC patients with small-duct PSCs or those younger than age 20.”
- Liver Problems with Inflammatory Bowel Disease