- News.Medical.Net: Study: Kissing after a gluten-filled snack is safe for people with celiac disease
- K Sullivan. NBC News 5/5/25: Can you kiss someone who just ate gluten if you have celiac disease? A study says yes
An excerpt from News Medical:
Researchers recruited 10 couples, each with one partner who has celiac disease, for a two-part study. In each session, the non-celiac partner ate 10 saltine crackers, and then the couple kissed for 10 seconds. In one session, the partners waited five minutes before the kiss, and in the other, they drank 4 ounces of water before kissing…
Although gluten was still found in saliva after kissing a partner who had consumed gluten and then had a glass of water, in all cases the amount was less than 20 parts per million, the level allowed in gluten-free products, which is considered safe.
“Patients with celiac disease can be more relaxed, knowing that the risk of gluten cross-contact through kissing a partner who has consumed gluten can be brought down to safe levels if food is followed by a small glass of water.”
From NBC article:
In the first scenario — waiting five minutes before kissing — two of the celiac participants had more than 20 parts per million of gluten in their saliva sample.
In the scenario in which non-celiac partners drank 4 ounces of water before the kiss, everyone’s saliva tests contained fewer than 20 ppm of gluten.
My take: Sounds like a fun study. Best to drink water before kissing your partner who has celiac disease.
Reference: Anne Lee. DDW Abstract Mo1242, 5/5/25: “Assessing gluten transfer via kissing; a prospective study of celiac-discordant couples”

- Ultra-Short Celiac Disease
- Celiac Disease: Pro Tips (Part 1)
- Celiac Disease: Pro Tips (Part 2)
- Celiac Disease: Pro Tips (Part 3)
- Celiac Disease: Pro Tips (Part 4)
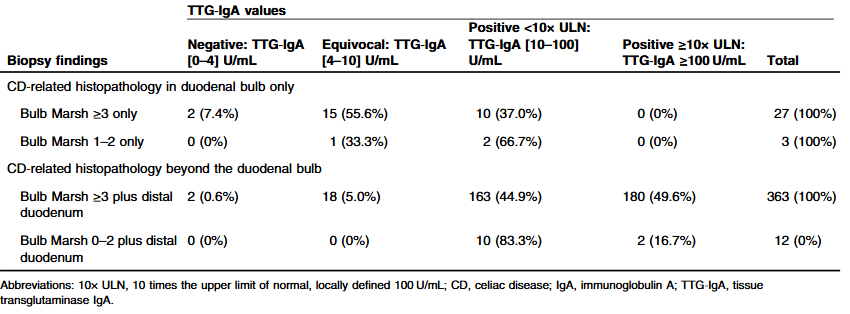
- How Many Children with Type 1 Diabetes and High Celiac Titers Have Celiac Disease
- “When is Celiac Disease Celiac Disease?”
- 2023 ACG Celiac Guidelines for Adult and Children
- Taking One ‘Bite’ At A Time -For Celiac Diagnosis | gutsandgrowth
- Celiac Disease: “”80 percent of success is just showing up” | gutsandgrowth
- What To Do For Pediatric Patients with Non-Responsive Celiac Disease
- Treatment of Refractory Celiac Symptoms with a Low FODMAP Diet
- Predicting Risk of Celiac Disease in High-risk Families
- Celiac Advocacy: Food Labeling Modernization Act
- Persistent Villous Atrophy in Celiac Disease Despite a Gluten-Free Diet
- Real-World = Partially-Treated Celiac Disease
- Best Screening For Celiac At All Ages
- Does The Degree of Villous Atrophy Affect Long-Term Outcomes with Celiac Disease? Plus One
- Study May Indicate Biologic Basis for Brain Fog in Persons with Celiac Disease
- @AmyOxentenkoMD: Celiac Disease and Mimics
- 99% Accuracy in Non-Biopsy Diagnosis of Celiac Disease