The proverb “Necessity is the mother of invention” is often attributed to Plato. In the dialogue of The Republic, Plato wrote, “our need will be the real creator”. This quote came to mind as I was reading about the use of f for fatigue in inflammatory bowel disease (IBD).
CD Moulton et al. Clin Gastroenterol Hepatol 2024; 22: 1737-1740. Open Access! Modafinil for Severe Fatigue in Inflammatory Bowel Disease: A Prospective Case Series
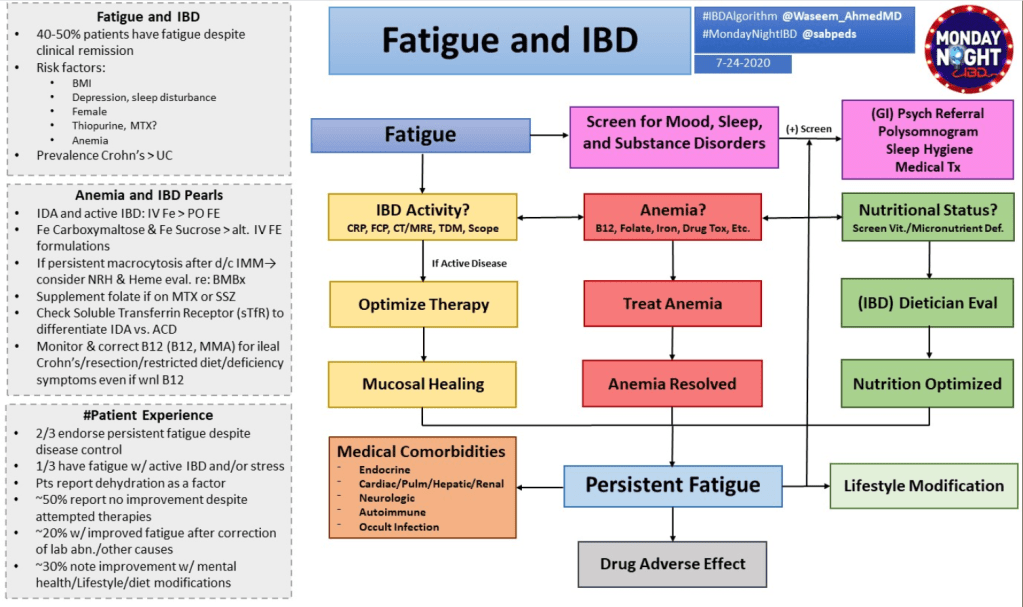
Background: “Fatigue is highly prevalent in patients with IBD, affecting 72% of patients with active inflammatory bowel disease (IBD) and 47% in remission, and is associated with poor quality of life, absenteeism and presenteeism.1 However, understanding the mechanisms of IBD fatigue remains limited, as reflected in a lack of effective treatments.1“
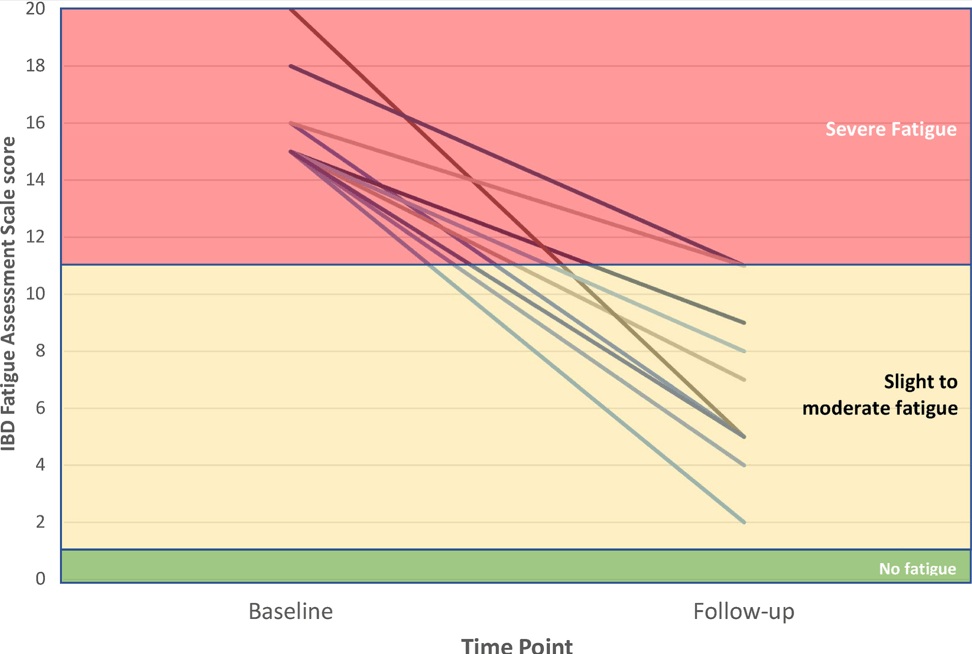
Methods: “Ten patients with IBD and severe fatigue were referred to a consultant psychiatrist. In all cases, mucosal inflammation and organic causes of fatigue (anemia, B12 deficiency, hypothyroidism) had been investigated and treated as much as possible. We measured fatigue severity using the IBD Fatigue Assessment Scale (IBD-FAS), designed specifically for IBD.5 Scores of 11 or higher out of 20 indicate severe fatigue and we only included patients scoring in this range.5
Dosing (for adults) of modafnil is described in the article.
Key findings:
- “At baseline, the mean IBD-FAS score was 16.0 (SD, 1.7) of 20. After modafinil treatment [at 6 months], the mean IBD-FAS score was 6.7 (SD, 3.0), representing a mean improvement of 58.1% from baseline.”
- “Although all 10 patients were severely fatigued at baseline, only 2 patients were still in the severe fatigue range after treatment.”
- “Tolerability was good: 1 patient reported transient headache and 1 patient reported transient dizziness; another patient reported mild palpitations; but none of the patients reported gastrointestinal side effects.”
My take: Perhaps, modafinil will be helpful –pharmacologic therapy for severe fatigue is an unmet need. More studies are needed as this is a small study without a control group.
Related blog posts: