Over the next 2 weeks or so, I am posting my notes/pictures from this year’s annual meeting. This post reviews the 2nd module from the postgraduate course.
This blog entry has abbreviated/summarized these presentations. Though not intentional, some important material is likely to have been omitted; in addition, transcription errors are possible as well.
Here is a link to postgraduate course syllabus: NASPGHAN PG Syllabus – 2017
Celiac Disease Diagnosis: ESPGHAN vs. NASPGHAN Guidelines
Michelle Pietzak Children’s Hospital of Los Angeles
This lecture started with a succinct history of celiac disease, including discussion of the banana diet and the observation that wheat deprivation during World War II was associated with improvement in children with celiac disease. The sequential diagnostic recommendations of ESPGAN and NASPGHAN were reviewed.
Key points:
- ESPGHAN 2012 guidelines separated children in two groups: symptomatic and asymptomatic. The guidelines indicated that symptomatic children with high titer serology (TTG IgA >10-fold ULN and positive EMA) could be diagnosed without an intestinal biopsy.
- ACG 2013 Guidelines: TTG IgA preferred serologic test if over age 2 years, TTG IgA along with deamidated gliadin (IgG and IgA) recommend if younger than 2 years. Even if negative serology, a biopsy was recommended if significant suspicion of diagnosis.
- NASPGHAN, AGA, ACG all recommend small bowel biopsy to confirm this lifelong condition
- The speaker did not critically discuss the Leonard et al study suggesting that 19% of individuals had persisting enteropathy on a gluten fee diet (see previous posts below)
- Jimmy Fallon: “10% of the population is allergic to gluten and 90% are tired of hearing about it”
Related posts:
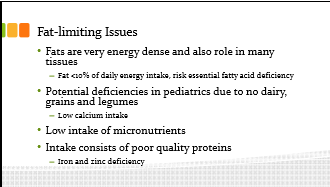
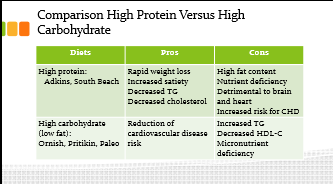
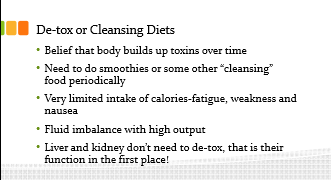
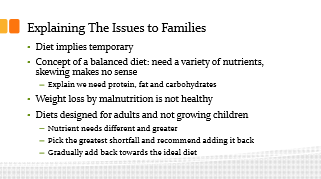
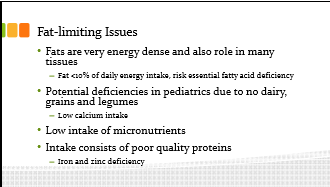
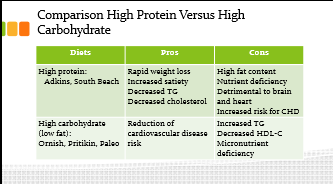
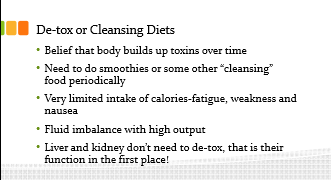
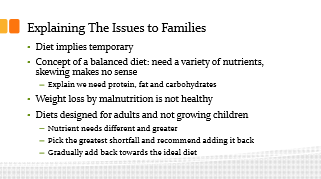
Fad Diets: The Good, the Bad, and the Just Plain Ugly
Mark Corkins University of Tennessee Health Science Center
Key points:
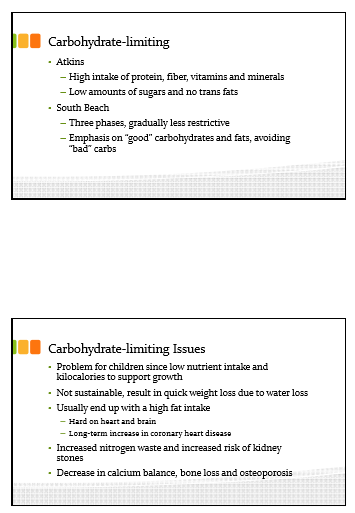
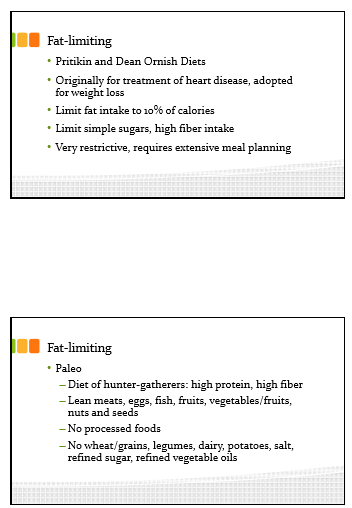
- Fad diets driven in part by obesity
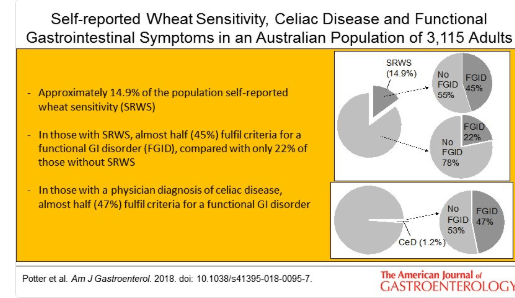
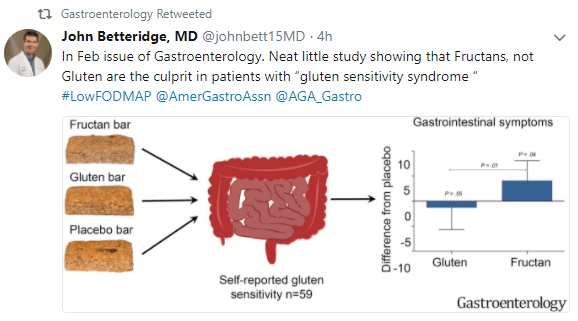
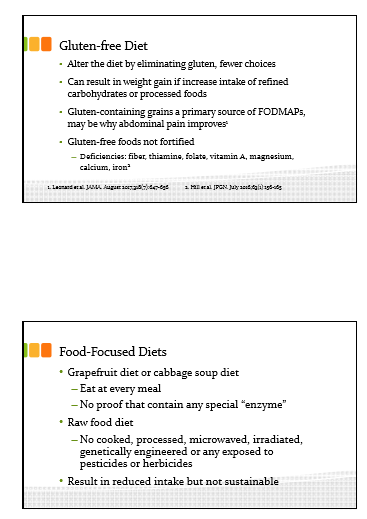
- Gluten-free diet is the most trendy, ~30% of U.S. adults are ‘limiting’ gluten, though most do not understand what gluten is. “Wheat Belly” book by Dr. William Davis has been influential despite lack of data.
- According to marketing report, 35% who consumer gluten limited diet have no reason for this, 26% for ‘healthier option,’, 19% for ‘digestive health,’, 13% for weight loss, 8% for gluten sensitivity
- Recommends: choosemyplate.gov. These feeding guidelines have been developed by nutrition experts.
Update on H pylori
Nicola Jones Hospital for Sick Children (Toronto)
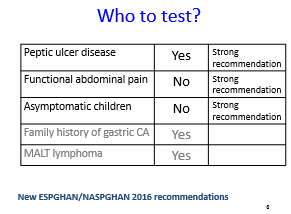
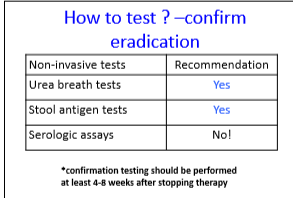
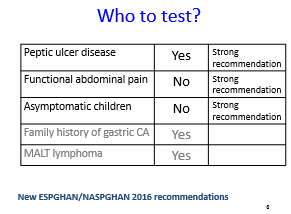
- Reviewed current recommendations based on ESPGHAN/NASPGHAN 2016 recommendations.
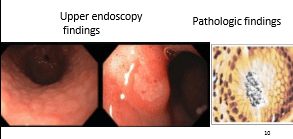
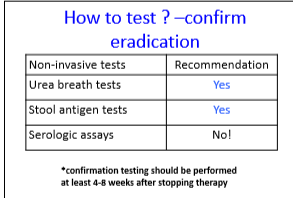
- The speaker indicates that upper endoscopy is recommended for initial diagnosis of H pylori but testing is not recommended for functional abdominal pain. The lecture did not address the issue that there can be an overlap in the presentations of these disorders.
- Adherence is crucial for adequate eradication
- Newer studies show improved eradication rates for quadruple therapy (bismuth-based) & in U.S. this is recommended as first-line treatment unless resistance patterns are known (which could allow for triple therapy)