M Egberg et al. AJC 2023: 118: 354-359. Low Risk of Lymphoma in Pediatric Patients Treated for Inflammatory Bowel Disease
Key finding:
- Using a database with 10,777 pediatric patients (2007-2018) with more than 28,000 patient years, there were 5 lymphomas reported. 4 had received thiopurines and none received anti-TNF monotherapy.
My take: This is a very reassuring study for the safety of anti-TNF agents.
AE Mikolajczyk et al. Inflamm Bowel Dis 2023; 29: 222-227. Assessment of the Degree of Variation of Histologic Inflammation in Ulcerative Colitis
- In this retrospective study with 92 patients (182 colonoscopies), the authors found “minimal variability between degree of inflammation among biopsy fragments within and among different colorectal segments in UC, suggesting that even a single biopsy would adequately reflect the inflammation of the entire colorectum.”
My take: This study suggests that taking biopsies from every segment of the colon (when it looks uniform) is usually not needed, unless the purpose is to look for dysplasia. Also, it is worth recognizing that individuals with primary sclerosing cholangitis often have greater histologic activity in the right colon.
References only:
- B Khosravi et al. Inflamm Bowel Dis 2023; 29: 42-50. A Practical Index to Distinguish Backwash Ileitis From Crohn’s Terminal Ileitis in MR Enterography
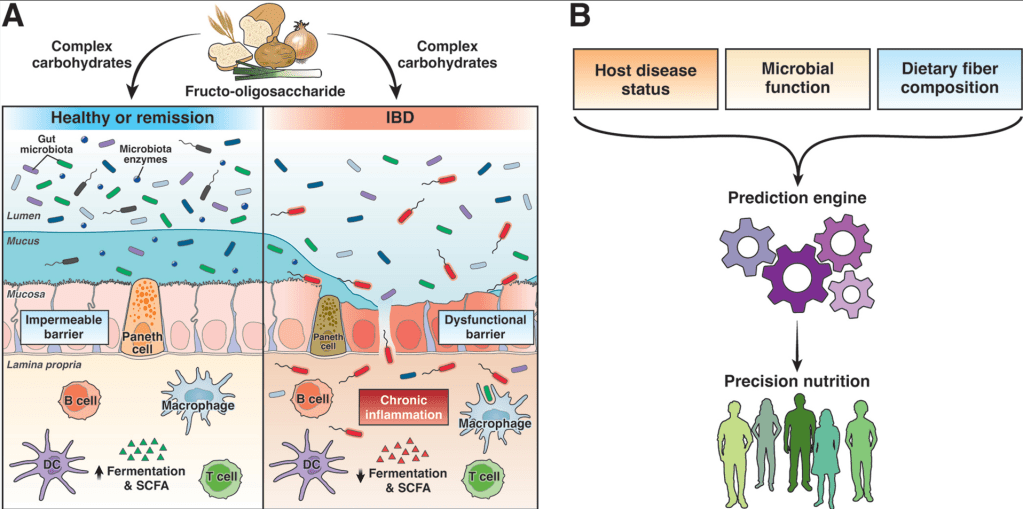
- HK Armstrong et al. Gastroenterol 2023; 164: 228-240. Open Access! Unfermented β-fructan Fibers Fuel Inflammation in Select Inflammatory Bowel Disease Patients
- Associated editorial to Armstrong Study: Gastroenterol 2023; 164: 182-184. Open Access! Promote or Prevent? Gut Microbial Function and Immune Status May Determine the Effect of Fiber in Inflammatory Bowel Disease