In June 2024 (special issue), Gastroenterology published an entire issue (193 pages) focused on celiac disease. There was a lot of useful information on almost every aspect of this disease. Below I have summarized some of the points.
ME Robert et al. Open Access! Opportunities for Improving Biopsy and Non–Biopsy-Based
Diagnosis of Celiac Disease
This article has the most pragmatic advice in the entire issue.
Key points regarding the Non-Biopsy Approach should be applicable in adults:
- “Retrospective studies in adults found that, in different clinical settings, TTG IgA raised to 10 or more times the upper normal value predicts the presence of mucosal atrophy from 95.2% in low-risk populations to 100% in high-risk populations. There is evidence that the magnitude of the TTG increase correlates with the risk of more severe damage at histology.”
- “A subsequent prospective multicenter, international study added further evidence for a non-biopsy approach. This study confirmed that a 5-fold and a 10-fold increase of TTG in a high-risk population predicted mucosal atrophy in 97.4% and 97.5%, respectively, when the biopsy was interpreted locally. However, after a central expert pathologist re-evaluated local histology, the PPV of a 10-fold TTG elevation was 99.4%…the only patient [without initial diagnosis of CeD] was eventually diagnosed as having CeD.”
- The authors discount the rationale for endoscopy in those with TTG IgA >10-fold ULN. 1. Missed CeD-related diagnosis (eg. EoE, lymphocytic gastritis): “The concern about missed endoscopic diagnoses in a biopsy-free approach appears to be a theoretical concern without empiric data.” 2. Concern for CeD complications: “Ulcerative jejunitis and enteropathy-associated T cell lymphoma are rare and, generally, not detected by the initial endoscopy” 3. Overdiagnosis (identification of Potential CeD):”PCeD is rarely found in cases of very high levels of TTG…Moreover, concern about the long-term implications of untreated PCeD may lead to a recommendation for a GFD, rendering moot the need for a biopsy.”
- Certain populations like those with type 1 diabetes should undergo a biopsy as the serology has a “lower specificity” in this group.
- There is concern that widespread adoption of a biopsy-free approach may lead to an over-reliance on serologies that fall short of the criteria that would lead to an accurate diagnosis.
Key points about Biopsy-Based Approach:
- At present, there is broad consensus that among individuals with an elevated TTG IgA that falls short of a 10-fold elevation, a biopsy-based approach is necessary.
- Obtain appropriate biopsies: guidelines recommend 2 biopsies from the first portion of duodenum and 4 biopsies from the distal duodenum (1 biopsy per pass recommended)
Related blog posts:
- No-Biopsy Approach to Celiac Disease Diagnosis and Positive Predictive Value (Based on Population)
- >99% Accuracy in Non-Biopsy Diagnosis of Celiac Disease
- The Non-Biopsy Diagnosis of Pediatric Celiac Disease
- “To biopsy or not to biopsy” –that is the question (for Celiac disease)
- Increased Risk of Irritable Bowel Before and After the Diagnosis of Celiac Disease
- Followup Biopsies in Pediatric Celiac Disease?
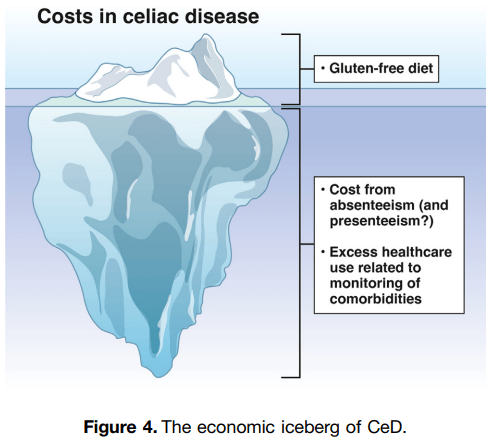
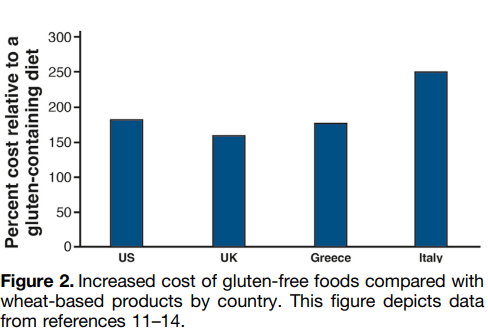
SR Bozorg et al. Open Access! The Economic Iceberg of Celiac Disease: More Than the Cost of Gluten-Free Food
Key points:
- Long-term data from Sweden have revealed a persisting excess use of health care, with health care costs estimated to be 1.79 times higher than in reference individuals up to 5 years after diagnosis. Similar observations were made by Violato et al, who found UK primary health care costs in patients with incident CeD to be approximately 1.9 times higher than in reference individuals from 5 to 10 years after diagnosis.
- Data collected from the Swedish national social insurance register showed that working-age patients with prevalent CeD had 1.49 times more work loss than matched reference individuals (42.5 days vs 28.6 days), equivalent to $2800 in lost productivity in 2015

Related blog post: Work Disability with Celiac Disease




