I have had the privilege of working with Olga for 26 years. She is a terrific physician and colleague. It is great that she is being recognized for her long-term commitment to her patients and the excellent care that she provides.

and Diane Benatar

I have had the privilege of working with Olga for 26 years. She is a terrific physician and colleague. It is great that she is being recognized for her long-term commitment to her patients and the excellent care that she provides.

Link: 2025 AAP Award Winners
I was unaware previously of the Mitchell B Cohen award. This early to mid-career leadership award was established in 2023. It is terrific that this award is available and named after Dr. Cohen (my mentor) who has done so much for our field.
Congratulations to Dr. Feldman and Dr. Di Lorenzo -this year’s AAP award winners.
S Karjoo et al. JPGN 2025;81:485–496. Evidence-based review of the nutritional treatment of obesity and metabolic dysfunction-associated steatotic liver disease in children and adolescents
This invited commentary reviews the data for several diets that may improve weight loss and metabolic dysfunction-associated steatotic liver disease (MSALD).
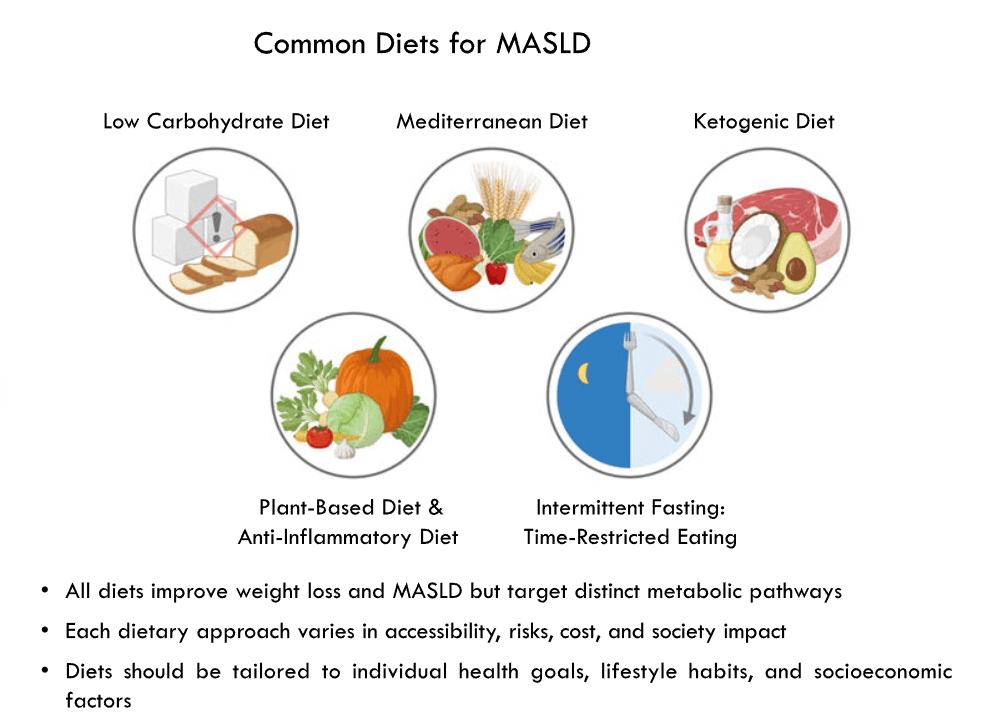
Several points:
My take: Each of the diets reviewed can help MASLD and obesity. Most patients pursuing dietary therapy would benefit from working with a nutritionist.
Related news: TEVA Press release, August 28, 2025: Generic liraglutide (need for daily injections) is now available.
Related blog posts:
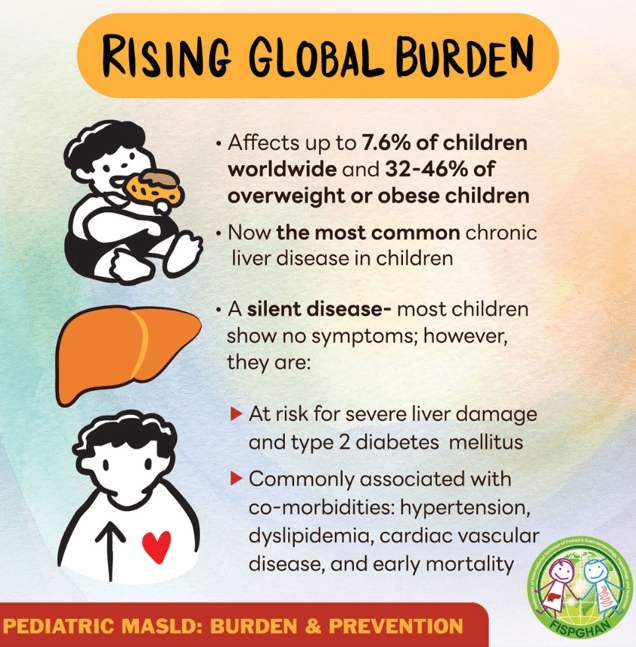
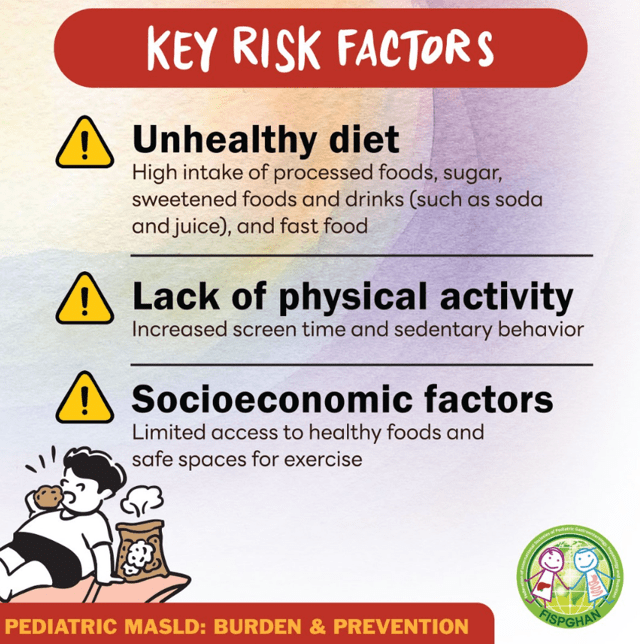
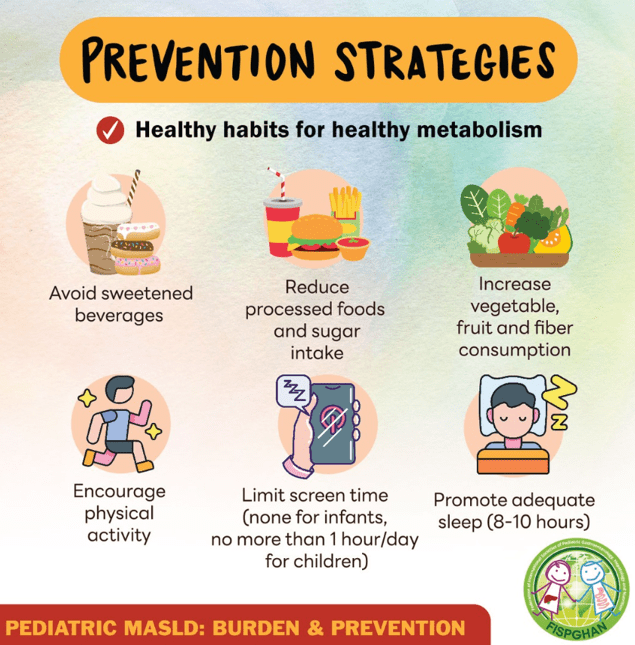
Also, related patient advice from Federation of International Societies for Pediatric Gastroenterology, Hepatology, and Nutrition (FISPGAN) –outlines risk factors and prevention tips for metabolic dysfunction-associated steatotic liver disease (MASLD):
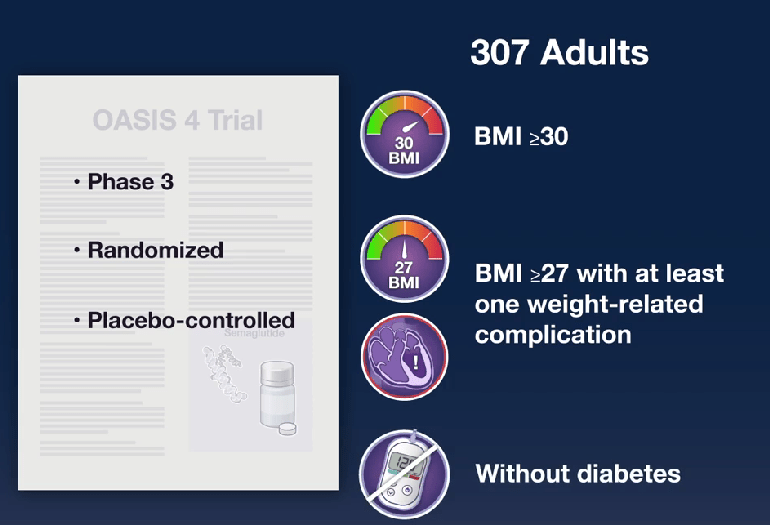
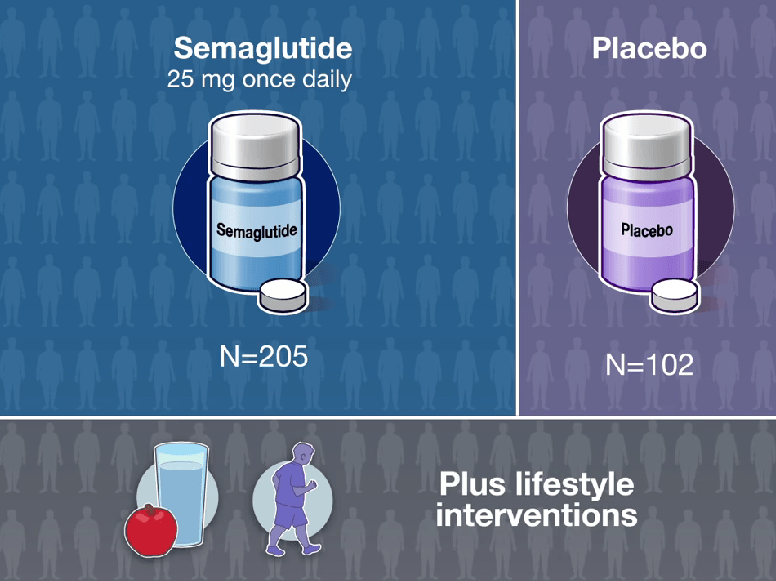
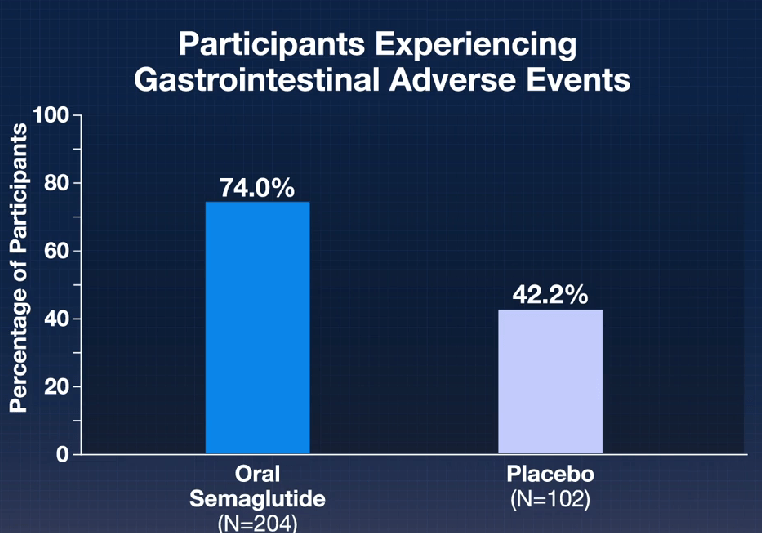
SWharton et al. N Engl J Med 2025;393:1077-1087. Oral Semaglutide at a Dose of 25 mg in Adults with Overweight or Obesity
Methods: The participants were randomly assigned in a 2:1 ratio to receive oral semaglutide (25 mg) or placebo once daily, plus lifestyle interventions.
Key Findings:
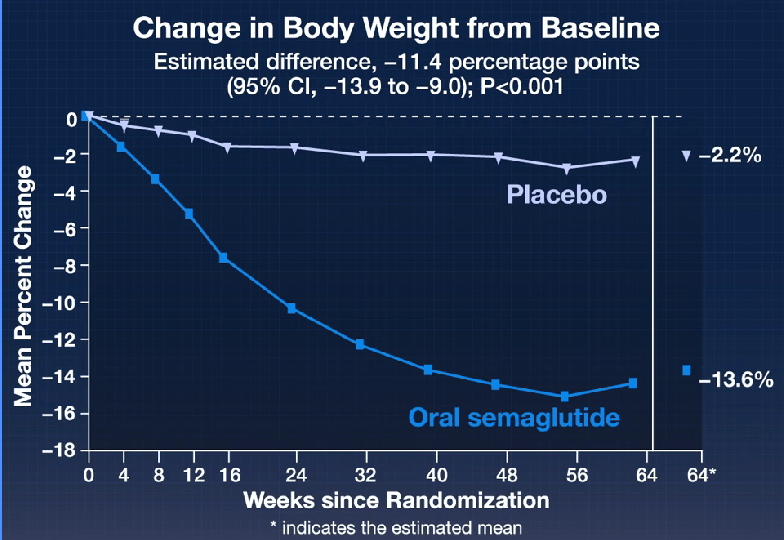
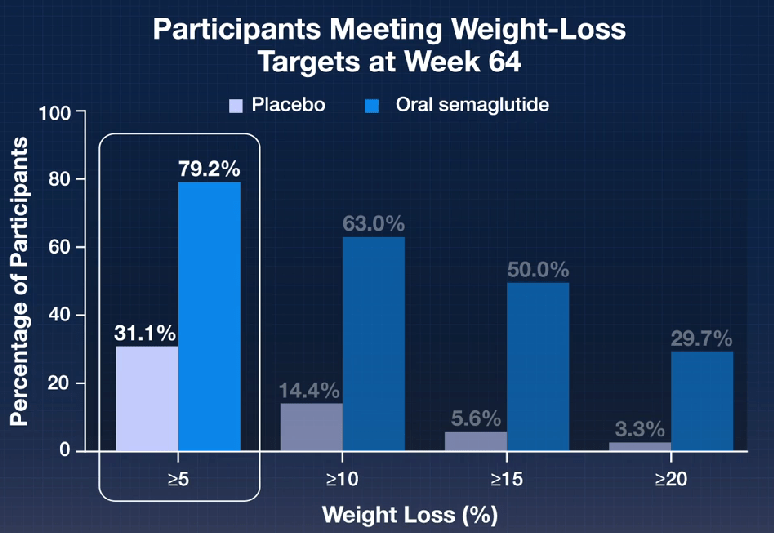
In their discussion, the authors note that the reasons why “patients may prefer oral administration over the subcutaneous route are most often needle aversion and local skin reactions.7,8 In addition, unlike injectable agents, oral agents may not require a refrigerated chain of delivery and could widen the reach of obesity care in many regions of the world where a lack of refrigeration represents a barrier to access.”
In addition, the results were similar to the “STEP 1 (Semaglutide Treatment Effect in People with Obesity) trial of weekly subcutaneous semaglutide at a dose of 2.4 mg (12.4 percentage points more than that with placebo),16“
As with prior trials of semaglutide, “treatment was also associated with substantial reductions in cardiometabolic risk factors including BMI, waist circumference, and levels of glycated hemoglobin, fasting plasma glucose, fasting serum insulin, lipids (very-low-density lipoprotein and triglycerides), and C-reactive protein.”
My take: Effective oral therapy is a big advance for management of obesity. The entire field of pharmacology for obesity has seen remarkable advances in the past few years. For me, it is reminiscent of the proliferation of published studies for hepatitis C around 10 years ago.
Related article in same NEJM issue: J Rosenstock et al. N Engl J Med 2025;393:1065-1076. Orforglipron, an Oral Small-Molecule GLP-1 Receptor Agonist, in Early Type 2 Diabetes
In the ACHIEVE-1 Trial: Key Findings (n=559 adults):
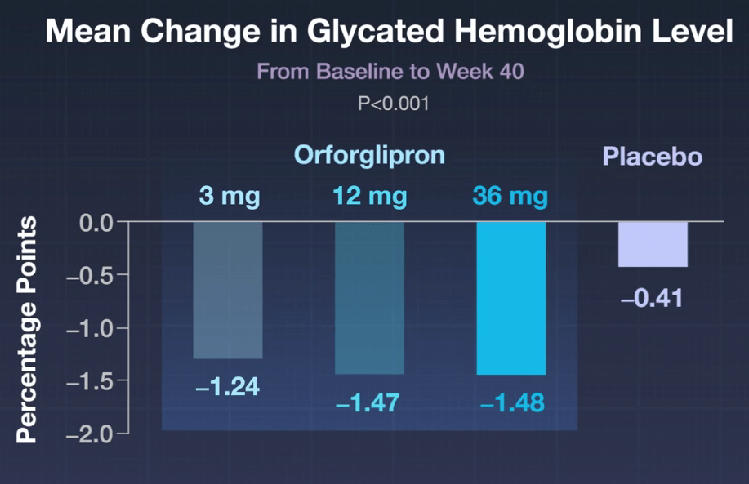
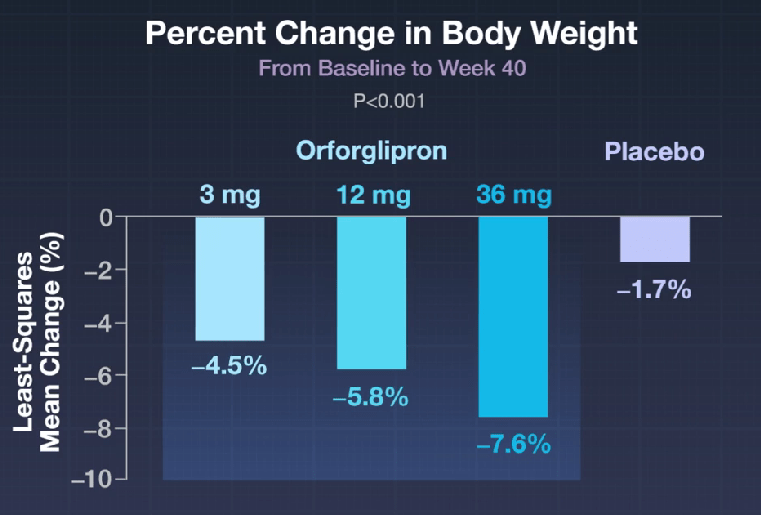
The associated editorial by DB Lowe (N Engl J Med 2025;393:1133-1134) notes that Orforglipron is a small molecule that manages to mimic the effects of glucagon-like peptide-1 (GLP-1) at the GLP-1 receptor. “The incretins, like many peptide hormones, are fairly small as proteins go — a few dozen amino acids long. But that makes them gigantic as compared with small-molecule drugs. Their molecular weights are at least 10 times as high as the 300 to 500 mass units that medicinal chemists have traditionally aimed for, and being peptides, they have generally undesirable properties as well. Many have short half-lives in the circulation, which can be a desirable feature for endogenous peptides but is nowhere near what is needed for the administration of a once-daily dose.”
Related blog posts:
S Lipstein. NEJM 2025; 393: 1249-1251. Insight into Corporate Governance — What Motivates Hospitals and Delivery Systems
This commentary provides a useful perspective on how hospitals view consolidation of health care. This article is one of many on the topic of corporatization of health care in recent NEJM issues. The author pushes back on the notion that the motivation is purely financial. And, the author argues that a lot of the concerns with poor outcomes/life expectancy despite high expenditures in health care actually are related mainly to poverty level, gun-related mortality, and public social services expenditures.
Here’s an excerpt:
Critics of such large-scale combinations argue that when clinical assets are aggregated within contiguous geographic areas, there is market consolidation. And market consolidation leads to anticompetitive behaviors, resulting in higher prices without concomitant quality improvements, fewer small innovative providers left to disrupt the status quo, and depressed wages for health care workers.
Delivery system leaders view asset aggregation in a different way — as a vehicle for efficient deployment of human, physical, and financial capital to achieve a health care mission. Upsizing by means of mergers and consolidation, hospitals and delivery systems realize benefits that come with economies of scale, spreading fixed operating costs…over a larger base of patient care revenue. Aggregating hospitals and physician practices within contiguous geographic areas enables systems to make large investments in facilities and technology that serve more people and avoid costly duplication….
Large-scale aggregation of health care delivery enterprises helps level the playing field with large-scale payers…
Often underappreciated is the importance for health systems of cultivating managerial bandwidth and subject-matter competencies unique to health care. As a health system grows, it gains the ability to compete on a national scale for top talent and expertise…
Use of the term “corporatization” suggests that health care mega-providers are money-motivated, focused on goals that are all about the bottom line. But money motivation in health care is not unique to big corporations…
In my experience, governing boards of delivery systems have four expectations of their executive leaders. Each expectation drives a financial motivation to generate the requisite revenues, operating margin, and investment capital.
First, to take good care of people when they are sick or injured and to help people remain as healthy… the delivery sector must have the financial capacity to invest in workforce skill development and training, renewal and expansion of patient care infrastructure and technology, and business and enterprise management systems…
Second, to operate in a financially responsible way, a delivery system needs to generate a positive operating margin, meaning revenues greater than expenses…
Third, to position a health care enterprise for long-term sustainability, it requires the financial fortitude to withstand the vagaries of economic and political cycles that might jeopardize the future availability of services…
And fourth, to stay true to a social or academic mission, many health care institutions make substantial financial commitments to their local communities and affiliated universities…
Comparisons of life expectancy and health spending are unadjusted for important differences among countries, including household income and poverty levels, gun-related mortality, and public social services expenditures.2,3 Nobody benefits if we ascribe poor health outcomes to corporatization and ignore true determinants…
Until we devise better solutions to improve the health of people whose economic disadvantages and behaviors reduce longevity, the United States will continue to lag.
My take: This article explains how health care systems view consolidation. Overall, my view is that the costs associated with hospitals are too high and some of this could be curtailed without affecting outcomes (see: When Hospitals Look Like The Ritz (But Cost Even More)).
Related blog posts:

LM Felipez et al. J Pediatr Gastroenterol Nutr. 2025;81:1100–1117. Open Access! North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition position paper on the therapeutic drug monitoring in pediatric inflammatory bowel disease
Therapeutic Drug Targets Based on Condition, Medication and Time of Therapy:
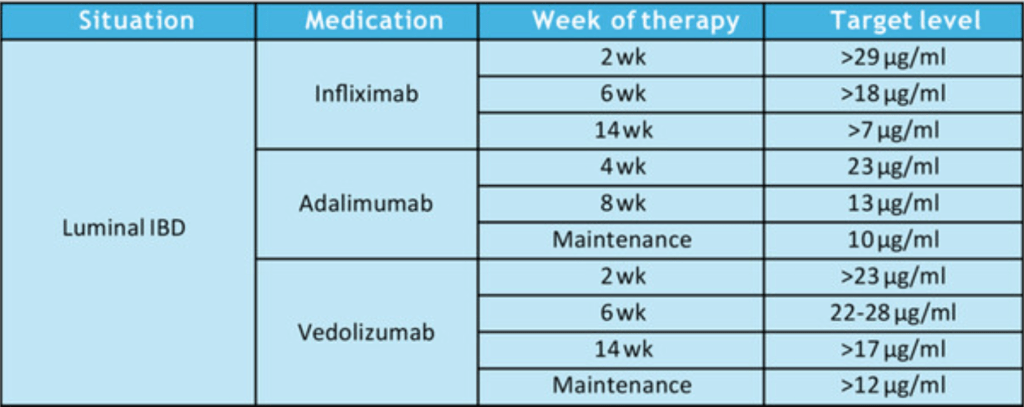
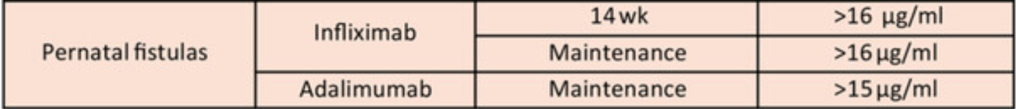
Discussion Points:
My take: “This NASPGHAN position paper should also serve to document that high-dose therapy, especially guided by TDM, is evidence-based standard of care.” This article clearly establishes three key points:
Related blog posts:
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.
G Lassailly et al. Clin Gastroenterol Hepatol 2025; 23: 1567-1576. Open Access! Resolution of Metabolic Dysfunction-associated Steatohepatitis With No Worsening of Fibrosis After Bariatric Surgery Improves 15-year Survival: A Prospective Cohort Study
Methods: From 1994 to 2021, 3028 bariatric patients at the University Hospital of Lille were prospectively included. Baseline liver biopsies were systematically performed with proposed follow-up biopsies 1 year after surgery, mainly in patients with MASH. We evaluated the association of the baseline and 1-year histologic progression of MASH and fibrosis status and long-term survival. The median follow-up was 10.1 years. At baseline, 2641 patients (89%) had a biopsy, including 232 with MASH (8.7%) and 266 (10.8%) with significant fibrosis (grade F2-F4). At 1 year, 594 patients had qualitative paired biopsies.
Key findings:
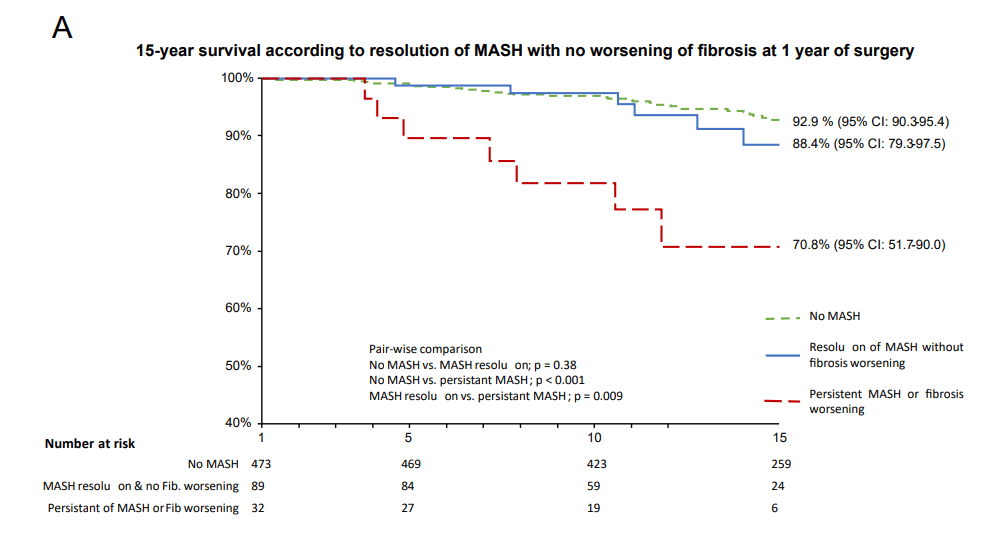
My take (borrowed in part from the authors): “This is the first study to show that the resolution of MASH with no worsening of fibrosis is associated with improved long-term survival.” Thus, histologic improvement is a very useful surrogate marker for long-term benefit in MASH, whether this is due to bariatric surgery as in this study but also with medical treatment.
Related blog posts:
Related News: Steve Gardner, USAToday 9/16/25: Legendary Dolphins QB Dan Marino reveals liver disease diagnosis
An excerpt:
In an interview with People magazine, the former Miami Dolphins quarterback said he first began feeling “a little fatigued” in 2007, and found out after a routine checkup that he had metabolic dysfunction-associated steatohepatitis, or MASH…
Marino, 64, says he now exercises more regularly than he did after his playing days ended. And he’s made major adjustments to his diet after doctors told him to “cut back on the wine and pizza and candy, ice cream, those kind of things.”
Nicholas Kristof, NY Times, 9/20/25: Trump’s Most Lethal Policy
Reporting from Uganda, Mr. Kristof reports on the devastating and worsening impact related to the cuts of foreign aid –without apparent cost savings. He details three particular avoidable deaths and outlines the larger problem. Here’s an excerpt:
The Trump administration has claimed that no one has died because of its cuts to humanitarian aid…Yet what I find here in desperate villages in southwestern Uganda is that not only are aid cuts killing children every day, but that the death toll is accelerating.
Stockpiles of food and medicine are running out here. Village health workers who used to provide inexpensive preventive care have been laid off. Public health initiatives like deworming and vitamin A distribution have collapsed. Immunizations are being missed. Contraception is harder to get. Ordinary people are growing weaker, hungrier and more fragile. So as months pass, the crisis is not easing but growing increasingly lethal — and because children are particularly vulnerable, they are often the first to starve and the first to die… credible estimates by experts suggest that the child death toll may be in the hundreds of thousands this year alone — and likely an even higher number next year.
A June 3 State Department memo, headed “sensitive but unclassified,” saying that the shutdown of the U.S. Agency for International Development will cost taxpayers $6.4 billion over two years… the money is necessary to manage “litigation, claims, residual payments and closeout activities.”..
A recent study published in The Lancet estimated that the cuts will cost the lives of about 690,000 children under the age of 5 in 2025, and 829,000 next year. The study estimated that some 3.1 million children under age 5 would die during Trump’s second term because of his cuts in humanitarian assistance...
PEPFAR, founded by President George W. Bush with the strong backing of America’s evangelical Christians. It turned the tide of AIDS and has saved 26 million lives — but the Trump administration has withheld some of its funding…About 65 percent of PEPFAR awards have been canceled…
Yet it’s also true that there are hints that the Trump administration is beginning to find some footing on aid. It has begun to place new orders for R.U.T.F. and has plans to move these stockpiles. It is preparing to hand over its food aid stockpiles to U.N. agencies to distribute to those in need. And it announced this month that PEPFAR will distribute lenacapavir, an important new drug that prevents AIDS transmission, in at least eight countries next year. These are real and positive steps; they just don’t make up for the larger pattern of chaos and cutbacks…
Related blog posts:

M Antaya et al. AJG; DOI: 10.14309/ajg.0000000000003733 (ahead of print); The impact of integrating pelvic MRI at diagnosis on early detection of perianal Crohn’s disease in pediatrics
Methods: “Patients [n=139] were prospectively enrolled into the Edmonton Pediatric Inflammatory Bowel Disease Clinic (EPIC) registry (baseline pelvic MR since 2018). A retrospective review (2018-2023) was performed.”
Key findings:
In their discussion, the authors indicate that pelvic MRI “enables identification of patients who may benefit from earlier biologic therapy (particularly anti-TNF) and closer monitoring despite being asymptomatic, given they have an increased risk of perianal surgery.” They note potential concerns for cost-effectiveness but note routine MRI may reduce future hospitalizations and surgery.
My take: In patients who will receive early biologic therapy, it is not likely that routine MRI will result in any cost savings. However, in settings without significant resource constraints, understanding the extent of disease is still desirable for later comparison.
Related blog posts:
Y Frutkoff et al. Gastroenterology 2025 (Article in Press). Open Access! Whole Food Diet Induces Remission in Children and Young Adults With Mild to Moderate Crohn’s Disease and Is More Tolerable Than Exclusive Enteral Nutrition: A Randomized Controlled Trial
Yesterday’s post (“A Practical Guide to Diet and IBD” (2025)) provided a summary of data on a multitude of diets for inflammatory bowel disease. Today’s post describes a study on a new diet, called the Tasty & Healthy diet.
Background: Tasty & Healthy (T&H) is a whole food diet for Crohn’s disease (CD) that excludes processed food, gluten, red meat, and dairy, without requiring formula or mandatory ingredients.
Tasty & Healthy (T&H) is an exclusive whole food diet, first published in a charity cookbook in 2014… The T&H diet was developed to reduce proinflammatory dietary exposures by excluding gluten, animal fat (ie, red meat and dairy, except for plain yogurt), as well as all processed food (anything that comes in a package except for those with 1 unprocessed ingredient.” (see details and supportive references in Supplementary Appendix 1).
Methods: TASTI-MM was a clinician-blinded, randomized controlled trial comparing tolerability and effectiveness of T&H (n=41) vs exclusive enteral nutrition (EEN, n=42). The intention to treat analysis included 83 patients (mean age 14.5 yrs, range 7-25 yrs).
Key findings:
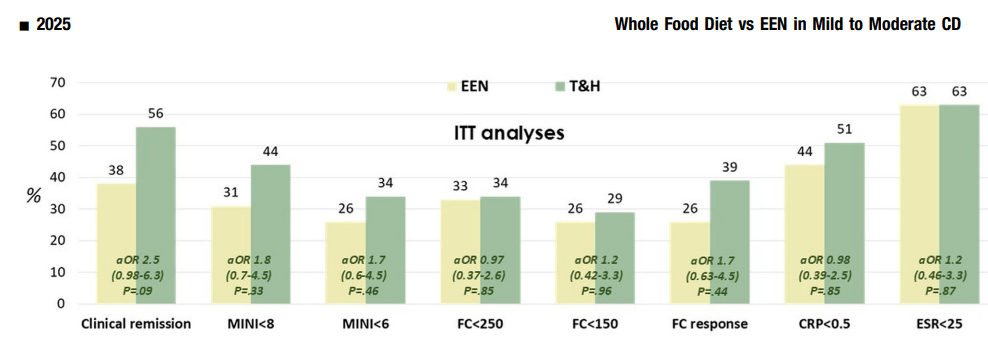
Discussion Points:
“In multiple studies CDED has been found to induce symptomatic remission in 62%–77% of patients with mild to moderate uncomplicated CD, including biologic remission in a subset of patients. Although conceptually similar to CDED in the exclusion of proinflammatory food
groups, the T&H diet differs in structure—requiring no formula and no mandatory components, thus offering greater dietary flexibility.”
“The T&H diet was tested across multiple international centers, while still achieving similar outcomes compared with EEN. The use of any exclusion diet requires guidance of a dietitian to ensure balanced nutrition, and this becomes even more important in diets when formula is not needed. Other exclusive whole food diets studied in the RCT setting are the Specific Carbohydrate Diet and Mediterranean diet, which were effective in inducing symptomatic remission, but demonstrated insufficient biologic remission rates.”
“In the past, dietary interventions have not been as widely adopted in adults as in children…Although EEN use has been hampered by the thought that adults will not tolerate nutritional interventions, the advent of whole food diets has changed that notion…In this study, we found that not only were the included adults adherent to the T&H diet, it was as effective as in children and treatment response was not associated with age.”
Related article: Plotkin L, Aharoni Y, Fenster D, et al. Tasty & Healthy is a
dietary approach for inducing and maintaining remission in Crohn’s disease: a prospective case series. United European Gastroenterol J 2021;9:521 (PO431).
My take: This “Tasty & Healthy” Diet appears to be an effective option for induction of remission for mild to moderate Crohn’s disease. Extended studies will be needed to help determine whether it could be used for longer duration in those with a response. Also, whoever labelled this diet initially clearly understands marketing as it sounds a lot better than EEN or CDED.
Related blog posts:
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition