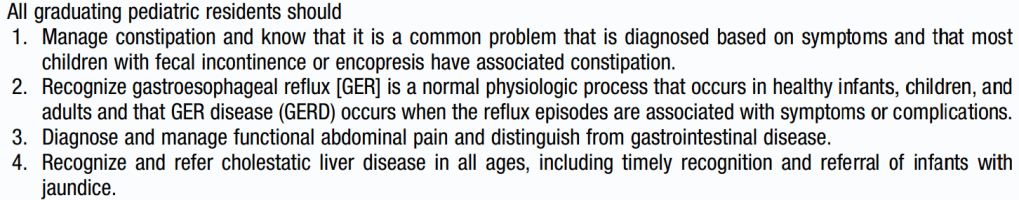
This blog entry has abbreviated/summarized these presentations. Though not intentional, some important material is likely to have been omitted; in addition, transcription errors are possible as well.
Here is a link to postgraduate course syllabus: NASPGHAN PG Syllabus – 2017
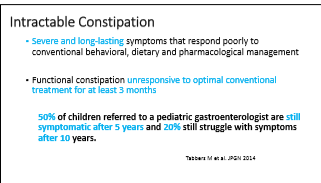
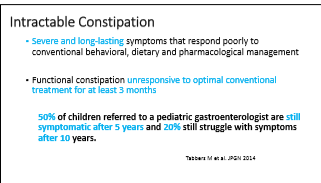
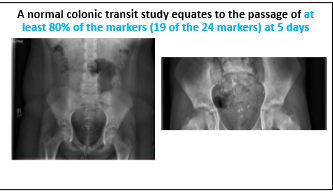
The child with refractory constipation
Jose Garza GI Care for Kids & Children’s Healthcare of Atlanta
Key points:
- Polyethylene glycol is a first-line agent and many patients require cleanout at start of therapy
- Adequate dose of laxative is needed for sure regular painless stools
- Don’t stop medicines before toilet training and until pattern of regular stooling established. “All symptoms of constipation should resolve for at least one month before discontinuation of treatment”
- Gradually reduce laxatives when improved
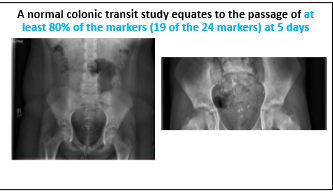
- An abdominal xray is NOT recommended to make the diagnosis of constipation
- Do you have the right diagnosis? Irritable bowel is often confused with constipation. With constipation, the pain is relieved after resolution of constipation.
- Outlet dysfunction. Stimulant laxatives (eg. Senna) are probably underutilized. Biofeedback may help in older children.
- Slow transit constipation. Newer prosecretory agents may be helpful –lubiprostone and linaclotide.
- Organic constipation. Hirschsprung’s, Spina bifida, anorectal malformations etc. Testing: anorectal manometry, rectal biopsy (for Hirschsprung’s)
- For refractory disease, consider rectal therapy –suppositories, transanal irritagations/enemas (~78% success for fecal incontinence/constipation). These treatments should be used prior to surgical therapy (eg. Malone antegrade continence enema/cecostomy)




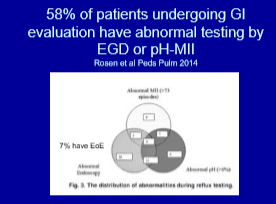
The quest for the holy grail: Accurately diagnosing and treating extraesophageal reflux
Rachel Rosen Boston Children’s Hospital
Key points:
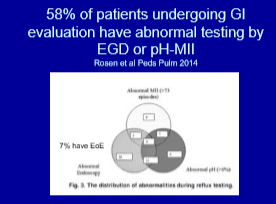
- It is frequent that EGD or impedance study will be abnormal, though this may not be causally-related.
- No correlation with ENT exams/red airways and reflux parameters
- No correlation with lipid laden macrophages and reflux parameters
- No correlation with salivary pepsin and reflux parameters
Treatment:
- Lansoprazole was not effective for colic or extraesophageal symptoms (Orenstein et al J Pediatrics 2009)
- PPIs can increase risk of pneumonia/respiratory infections
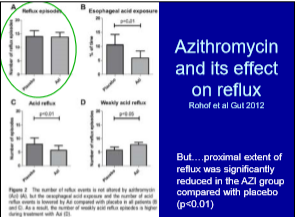
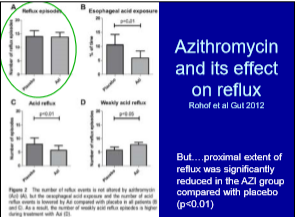
- Macrolides have been associated with increased risk of asthma but may be helpful for pulmonary symptoms
- Fundoplication has not been shown to be effective for reducing aspiration pneumonia. Fundoplication could increase risk due to worsened esophageal drainage.
- ALTEs (BRUEs -brief resolved undefined events) need swallow study NOT PPIs

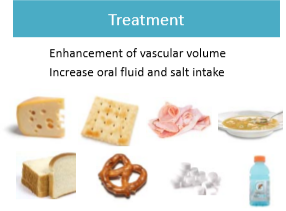
POTS and Joint Hypermobility: what do they have to do with functional abdominal pain?
Miguel Saps University of Miami
Key points:
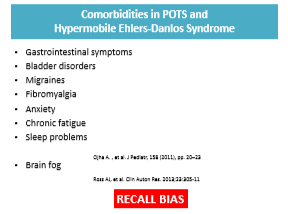
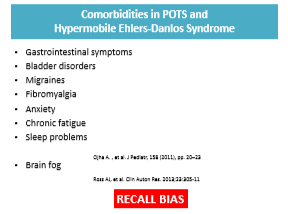
- Patients with POTS and joint hypermobility have frequent functional abdominal pain as well as other comorbidities
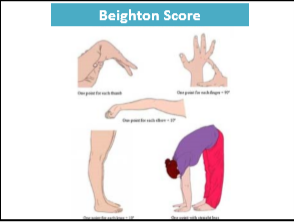
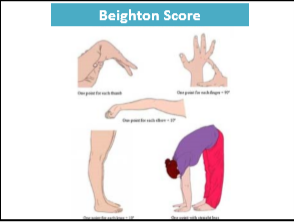
- Beighton Score can determine if joint hypermobility is present
- Brighton Score determines if hypermobile Ehlers-Danlos syndrome is present
- Patients with frequent fatigue. Gradual progressive and regular exercise is important part of therapy. Can start with recombant exercise – training bicycle exercise, swimming
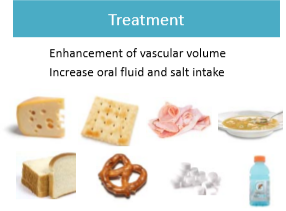
- Need to push salt intake and fluds

Do I need to test that C.R.A.P.?
Rina Sanghavi Children’s Medical Center Dallas
This basic talk reviewed a broad range of issues related to functional abdominal pain.
Key points:
- Carnett’s sign can help establish abdominal pain as due to abdominal wall pain rather than visceral pain
- What is an appropriate evaluation? Limited diagnostic testing for most patients.
- Alarm symptoms include: Fevers, Nocturnal diarrhea, Dysphagia, Significant vomiting, Weight Loss/poor growth, Delayed Puberty, and Family history of IBD