Douglas Wolf -New Treatments and New Strategies
- More proactive approach is recommended; this leads to less surgery, less hospitalization, and less antibodies to infliximab
- Risk assessment should guide treatment; higher risk indicates a need for more aggressive therapy
- Higher doses of anti-TNFs appropriate in some cases (eg weekly Humira)
- For distal colitis/proctitis, budesonide foam is an alternative to cortifoam
- Azathioprine monotherapy has a low response rate
- Combination therapy may not be needed if good IFX levels obtained. Though, it is possible that development of antibodies precludes achieving good levels; thus, combination therapy may increase likelihood of good levels by reducing antibody formation, particularly earlier in course
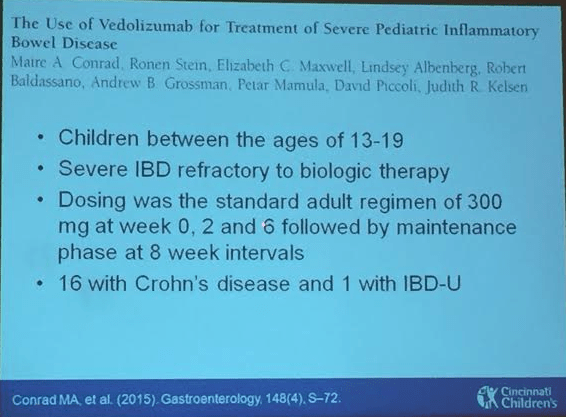
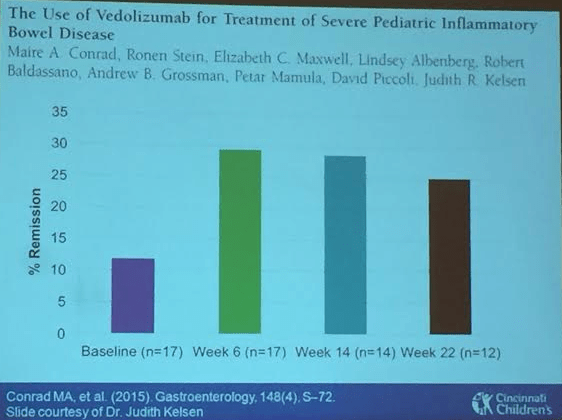
- Vedolizumab can be shortened to q4weeks if not improving.
- CALM study: symptom based management compared to management based treat-to-target relying on CRP, and calprotectin. Improved outcomes with treatment based on CRP, calprotectin in addition to symptoms.
- Tofacitinib –will be available in 2018 for ulcerative colitis
Chiristina Ha -Treatment Strategies in the Elderly
Dr. Ha referenced Dr. Sandborn who recently stated that combination therapy should be first-line therapy in moderate-to-severe disease –though this may be different in elderly patients.
- Older age –increases mortality risk
- Immunosenescence -relative immunodeficiency state associated with aging
- Pharmokinetic changes with aging
- Increased susceptibility to drug toxicity (eg. Renal, hepatic)
- Older patients usually excluded from therapeutic trials
- Polypharmacy is more common
Treatment:
- Frequent strategy in elderly has been using 5-ASAs and steroids, even in moderate-to-severe disease. This has been due to increased fear of adverse events with IMM and anti-TNFs. However, using data from rheumatoid arthritis, older patients’ biggest risk is steroids.
- Thiopurines have unfavorable risk profile in the elderly.
- Anti-TNFs are not as effective in the elderly
- Preliminary data on vedolizumab -very limited data, may work better in older patients
- Most common infections by be reduced considerably by immunizations. (eg. ,bacterial pneumonia, herpes zoster)
- Correct anemia, nutritional deficiencies
Disclaimer: These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) and changes in diet should be confirmed by prescribing physician. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.