Stephanie Nolen, NY Times 6/25/25: Kennedy Withdraws U.S. Funding Pledge to International Vaccine Agency
An excerpt:
The United States will withdraw its financial support of Gavi, the global organization that helps purchase vaccines for children in poor countries, Robert F. Kennedy Jr., the United States secretary of Health and Human Services, told the group’s leaders on Wednesday, accusing them of having “ignored the science” in immunizing children around the world…
“Any decision made by Gavi with regards to its vaccine portfolio is made in alignment with recommendations by the World Health Organization’s Strategic Advisory Group of Experts on Immunization (SAGE), a group of independent experts that reviews all available data through a rigorous, transparent and independent process,” Gavi’s statement said…
Dr. Atul Gawande, a surgeon who led global health work in the Biden administration, called Mr. Kennedy’s remarks “stunning and calamitous…”
The United States was the largest donor to Gavi, whose work is estimated to have saved the lives of 17 million children around the world over the past two decades…
Gavi had hoped to raise $9 billion for the 2026-30 period, funds the organization said would allow it to purchase 500 million childhood vaccinations and to save at least eight million lives by 2030. ..
The decision to end U.S. support for Gavi — which was included in the rescission package passed by Congress and now being considered by the Senate — leaves the organization with an immense hole in its budget…The Gates Foundation is maintaining its funding at a stable level from previous years — about $350 million in each of the next four years — as is the United Kingdom.
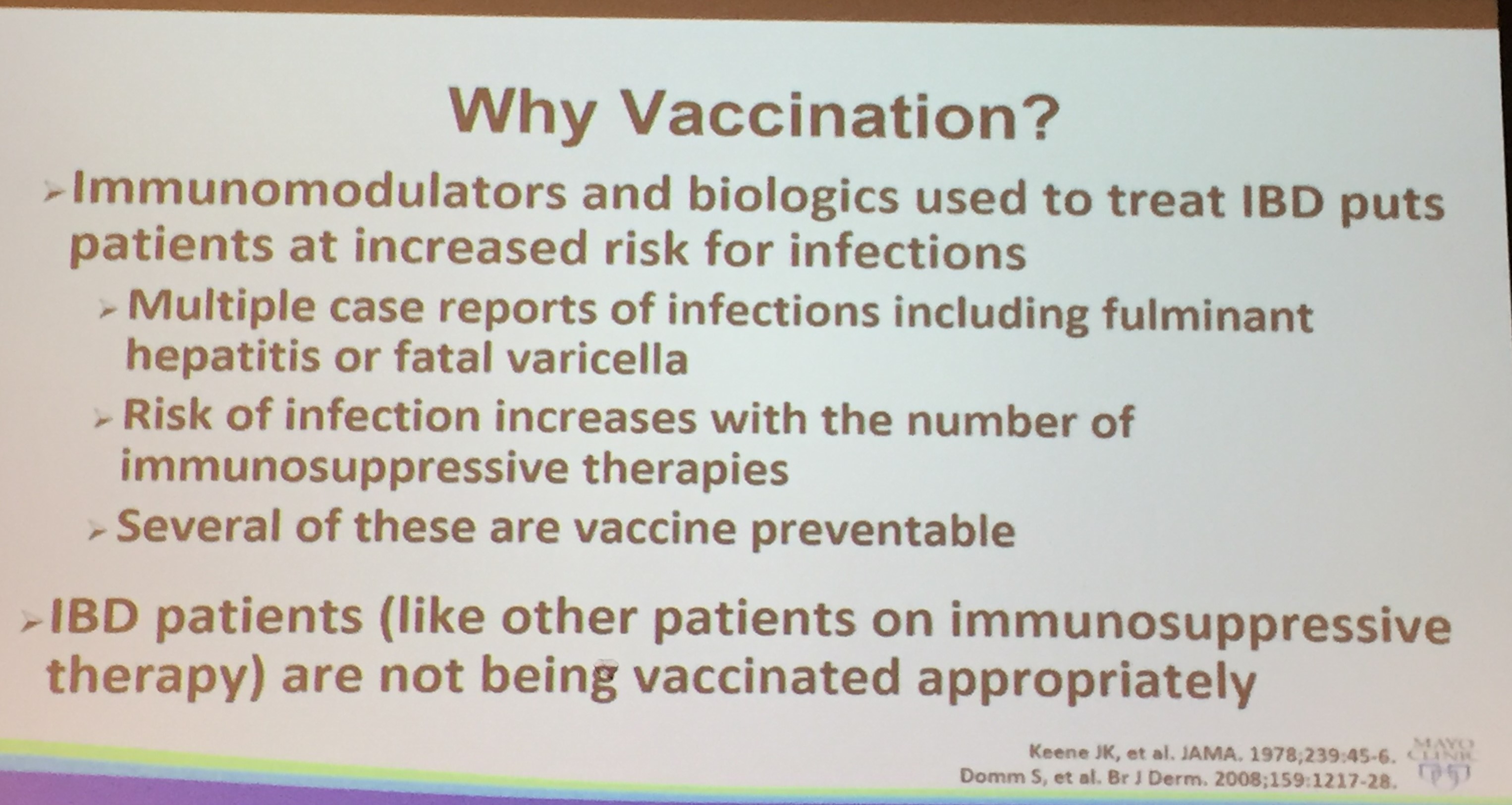
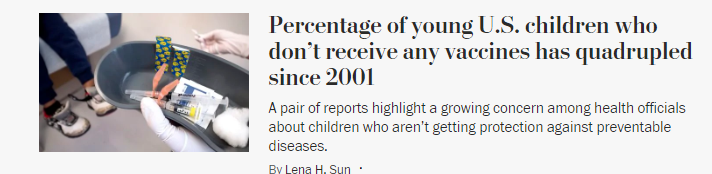
My take: It is no exaggeration to say that the shift in U.S. vaccine policy may result in hundreds of thousands of deaths every year. In addition, U.S. travelers will be more likely to be exposed to vaccine-preventable illnesses as well.
Related blog posts: