H Pearson, Nature, 6/24/25: Partly Open Access! How to make America healthy: the real problems — and best fixes
An excerpt:
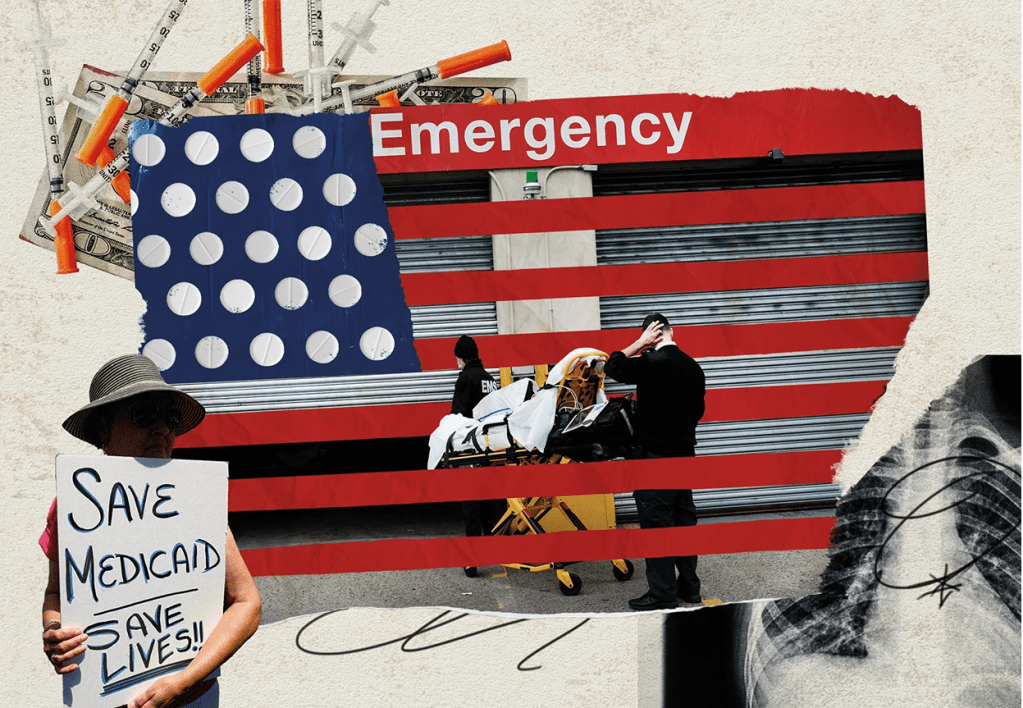
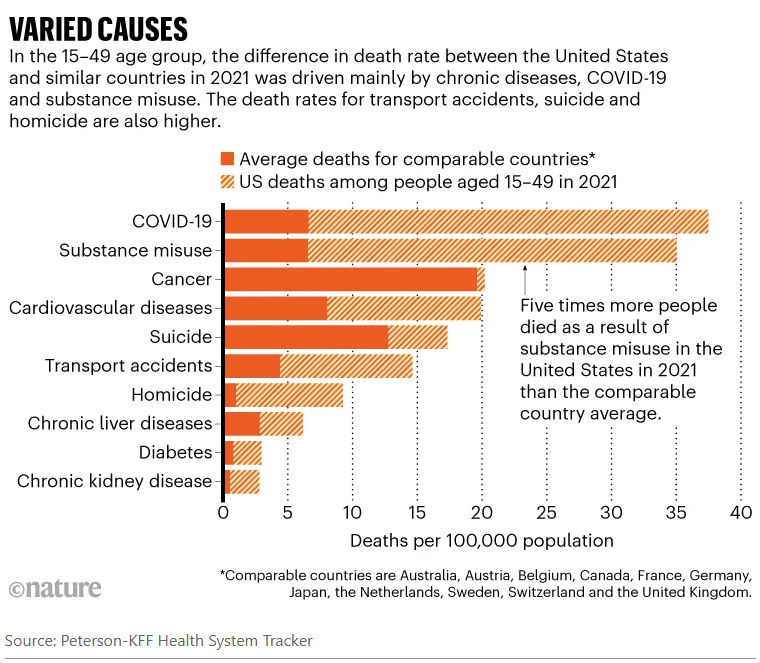
Since taking over as the top US health official in February, Robert F. Kennedy Jr has overseen radical changes that have alarmed many public-health experts…His mission, he says, is to ‘Make America Healthy Again’. “We are the sickest nation in the world,” he said in March, “and we have the highest rate of chronic disease.” His diagnosis holds some truth, say public-health specialists and analysts. Relative to other similarly wealthy nations, the United States has the shortest life expectancy despite spending the most on health care…And researchers agree that high rates of chronic disease, including heart disease and obesity, are key contributors to Americans’ higher death rates, as Kennedy emphasizes.
But researchers say that Kennedy — widely known as RFK Jr — has mostly ignored other leading causes of death and ill health, including car accidents, drug overdoses and gun violence…
Life expectancy in the United States was closer to the average for its peers around 1980 and gradually improved, according to KFF’s analyses. The gains were driven partly by a drop in smoking and increased use of cholesterol-lowering drugs known as statins…
Overall, chronic conditions — heart disease, cancer, stroke and respiratory disease — take up four out of five spots on the country’s list of biggest killers…One of the biggest drivers of those deadly conditions is obesity, say researchers. As of 2022, about 42% of adults were considered obese in the United States, compared with 27% in the United Kingdom and 5.5% in Japan. Obesity increases the risks of developing diabetes, heart disease, cancer and many other conditions. “The US has, particularly around diet, obesity and overweight, adopted unhealthier lifestyles at a higher rate than our country peers,” Bollyky says…
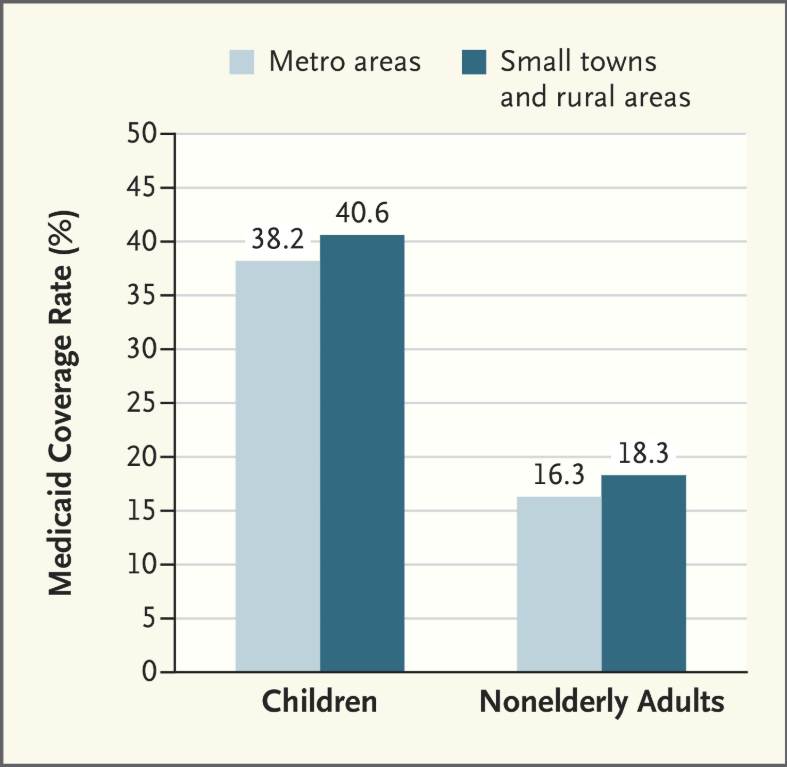
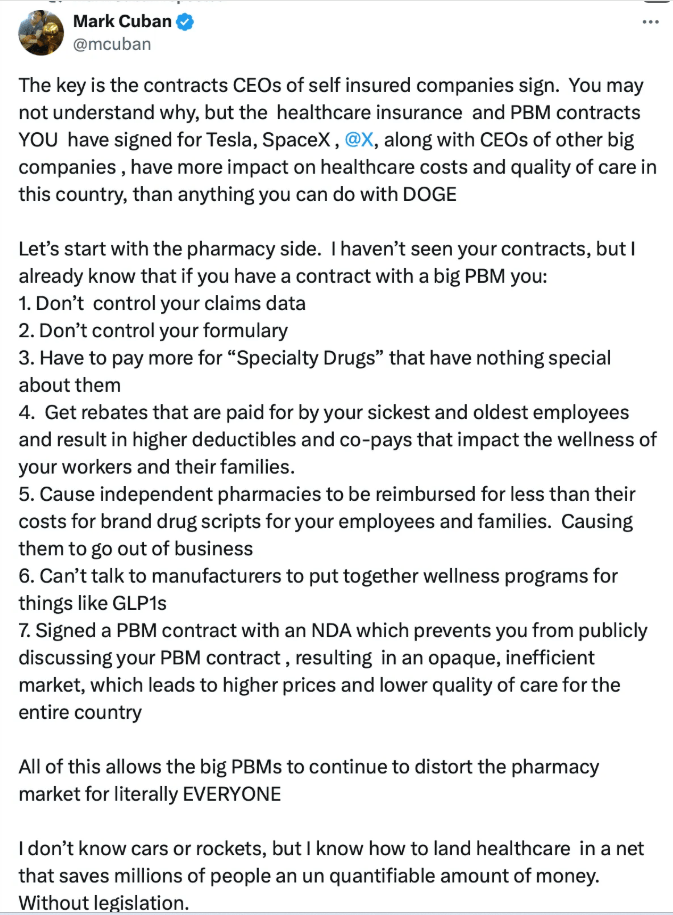
The problems caused by chronic disease are compounded by poor health care. Compared with a group of similar high-income countries, the United States is the only one that lacks universal health-insurance coverage… Lack of health insurance, high costs and other barriers prevent people from getting diagnoses and treatment early on…
The other big contributors to lower life expectancy in the United States — and what really sets the country apart, researchers say — are high death rates from substance misuse, car accidents, suicide and homicide (see ‘Varied causes’). These tend to kill people of working age…All told, the death rates in working-age people mean that one 5-year-old out of every 20 — or roughly one in every school class — will die before the age of 45, according to Angus’s calculations. The comparable figure is one in 50 in the United Kingdom and one in 100 in Switzerland…
Health spending in the United States was about US$13,000 per person in 2023, according to a KFF analysis. That compares to an average of about $7,000 per person in similar large, well-off countries…
Boosting rather than cutting spending on disease prevention is “where the big gains are
to be made on population health” [Reginald Williams, a health-policy specialist at the Commonwealth Fund says his] first priority would be to expand health coverage. In the United States, around 8% of people lack health insurance, compared with around 1% or less in similar high-income countries. The second, he says, would be to invest more in primary care — the physicians and other health professionals who are the first port of call for patients, and who deal with disease prevention and management…
Tackling the high death rates from overdoses and guns, meanwhile, would involve
addressing entrenched social and political issues such as gun ownership, poverty,
unemployment and inequality.
My take: Despite big promises from politicians, there are no quick fixes for improving our national health. Improving health care access would help but this does not address deaths due to firearms, drug overdoses and to car accidents.
Related blog posts:
- Longevity Gap Present Even in Wealthy Americans
- Ten Americas: Examining Health Disparities and Life Expectancy
- “Proposed Medicaid Cuts Could Lead to Thousands of Preventable Deaths Annually” & Personal Message
- How Putting America First is Undermining Health Outcomes Here and Globally
- No Exaggeration: Too Many Children Are Dying in the U.S.
- Firearms: #1 Cause of Pediatric Deaths & Households with Guns =More Deaths
- New study finds 45,000 deaths annually linked to lack of health …
- U.S. Health System: ‘World Leader in Amputations’
- Life Expectancy Dropping in U.S. (post in 2023)
- Zip code or Genetic code -which is more important? gutsandgrowth
- “More Than Half a Million Extra Deaths” Every Year In U.S.
- RFK Jr. Ousts Entire CDC Vaccine Advisory Committee
…