- U Bonnet. Gastroenterol 2024; 167:1054-1055 (letter). Cannabis Hyperemesis Syndrome Recovers Completely When the Use of Cannabis or Synthetic Cannabinoids Is Permanently Discontinued—Cyclic Vomiting Syndrome Does Not
- ME Mullins et al. Gastroenterol 2024; 167: 1055-1056 (letter). Comments on the AGA Clinical Practice Update on Diagnosis and Management of Cannabinoid Hyperemesis Syndrome
- AGA Clinical Practice Update (open access PDF): AGA Clinical Practice Update on Diagnosis and Management of Cannabinoid Hyperemesis Syndrome: Commentary (related blog post: AGA Practice Update: Cannabinoid Hyperemesis)
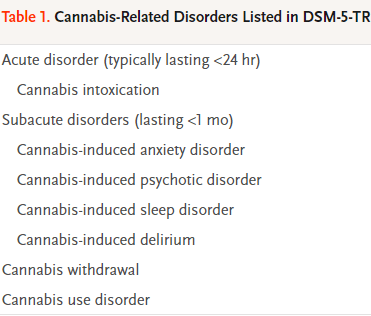
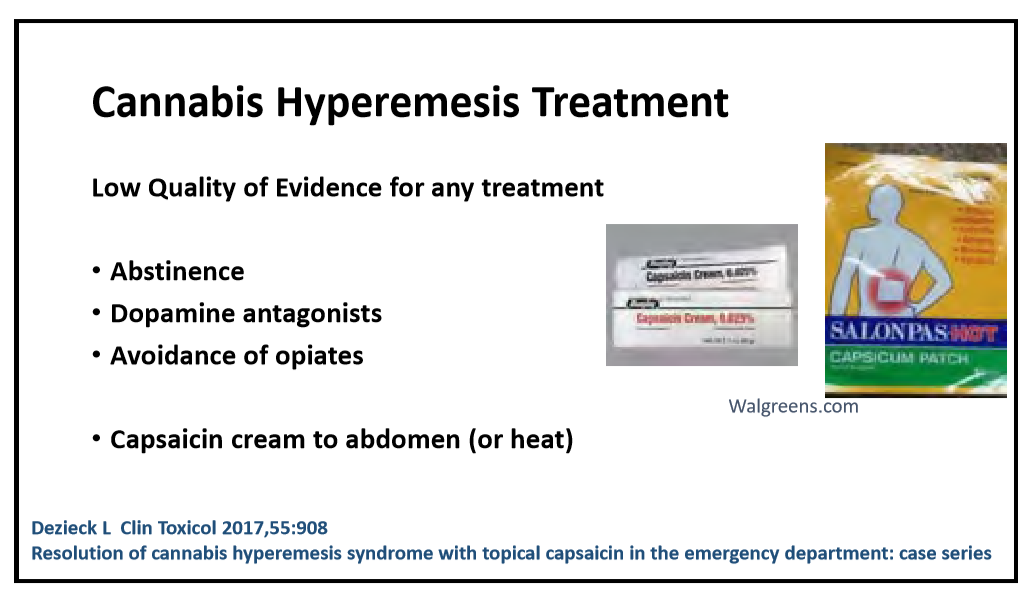
The correspondence regarding AGA’s clinical practice update on Cannabinoid Hyperemesis Syndrome offered a few useful points.
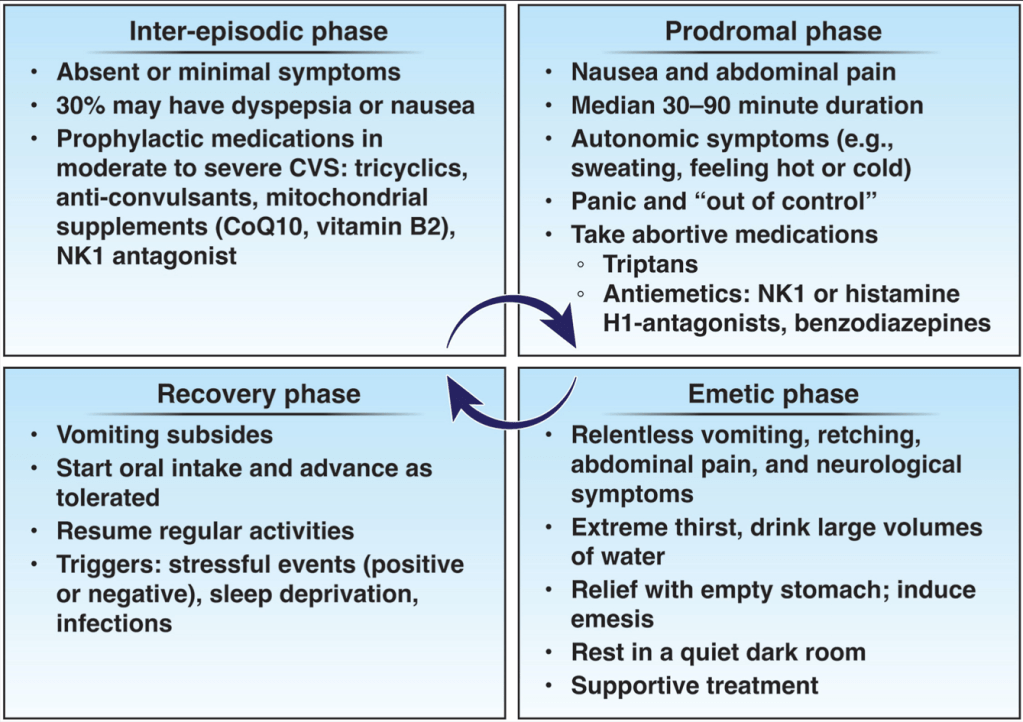
Bonnet notes that “CVS is most likely present if cyclic vomiting persists, recurs or worsens during cannabis abstinence (beyond 3-week cannabis withdrawal period, which may be temporarily accompanied by nausea). In other cases with more fluctuation symptoms, a clear distinction between CHS and CVS is not so easy…Evidence shows that a symptom-free period of about 12 months after cessation of long-term cannabis use should be sufficient to clearly distinguish CHS from CVS…Finally, I emphasize here that…CHS…in exceptional cases can lead to life-threatening conditions (eg due to prerenal failure, severe electrolyte disturbances, or esophageal rupture)…but recovers completely when affected patients permanently stop using cannabis or THC analogues.
Mullins et al note that “ondansetron is uniformly ineffective and that butyrophenones (haloperidol, droperidol) are more effective” for CHS. In the reply, the authors note that the data supporting these medications is based on small studies and some patients have developed acute dystonia.
Related blog posts:
- Cannabis Toxic Effects
- Does Stopping Cannabis Improve Cyclic Vomiting Syndrome?
- Legalized Cannabis Associated with Increased Vomiting and Dependency But What About Alcohol?
Images from “Chalktoberfest” in Marietta 10/11/24-10/13/24. The drawings are amazing, including some that appear to be 3-D: