N Ravanbakhsh et al. JGPN 2024; https://doi.org/10.1002/jpn3.12368. Comparing imaging modalities in the assessment of fibrosis in metabolic dysfunction-associated steatotic liver disease

Key findings:
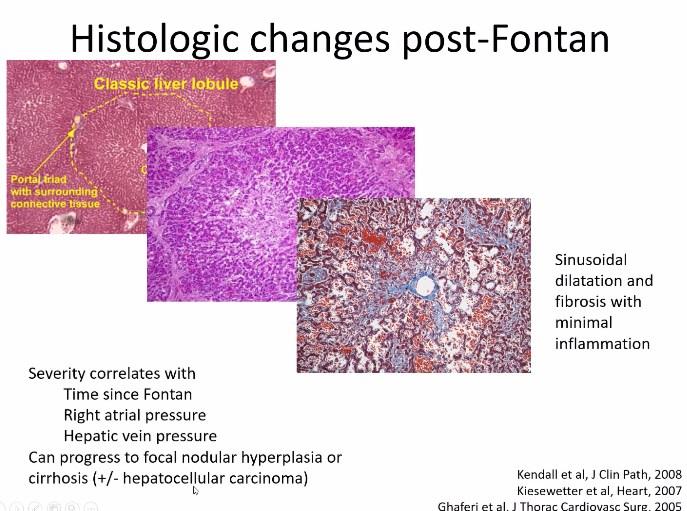
- TE and MRE did not have high correlation with liver biopsy in the detection of high-grade fibrosis
- Fibrosis was identified in 90% of liver biopsies with bridging fibrosis in 15 (19%) and cirrhosis in 1 (1%)
- AUROC curves of MRE and TE for detection of high-grade fibrosis were 0.817 and 0.750, respectively, and not significantly different.
The authors note that previous adults studies suggest that MRE is more accurate in the identification of liver fibrosis than TE (MRE detected ≥ F1 fibrosis with an AUROC of 0.82, while TE detected fibrosis with an AUROC of 0.67).20
My take: Trying to identify accurate non-invasive testing is crucial to help identify patients most in need of treatment and for limiting costs.
Related blog posts:
- Transient Elastography in Pediatric Liver Disease
- Briefly Noted: Progression of Fatty Liver Disease on MRI
- Increasing Prevalence of Steatotic Liver Disease in Adolescents