M Plassmeyer et al. Journal of Allergy and Clinical Immunology 2025; Dupilumab Opens a Therapeutic Window in Food Protein Induced Enterocolitis Syndrome by un-licensing dendritic cells
Thanks for Ben Enav for this reference.
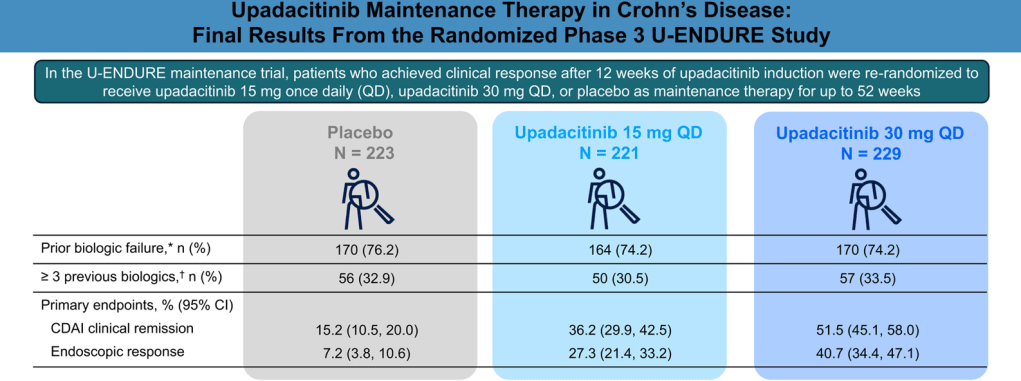
Methods: This was a two-part study: “(i) a detailed single-patient case of wheat-triggered, endoscopy-confirmed colitic FPIES treated with dupilumab 300 mg subcutaneously every two weeks and (ii) a prospective follow-up of seven additional FPIES patients all of whom initiated dupilumab for approved comorbidities. Serial flow cytometry quantified dendritic-cell OX40L and CD8+ CRTH2+ T-cell subsets before and after treatment; open food challenges assessed clinical tolerance.”
Key Findings:
- Index case: Within two injections of dupilumab, the wheat sensitive patient tolerated a 50 g wheat protein challenge without gastrointestinal symptoms—this was the first uneventful exposure in 20 years. Discontinuation of dupilumab led to relapse; re-initiation again restored clinical tolerance
- Cohort: All seven additional patients (ages 2–58 yr; triggers: milk, soy, rice, wheat, shellfish) achieved unrestricted dietary tolerance within three months
- An important finding in the index case as well as the follow up cohort is the dupilumab induced drop in dendritic cell OX40L. OX40L is a TNF-superfamily co-stimulatory molecule induced on dendritic cells and other antigen-presenting cells.
My take: Dupilumab appears to be a promising medication for FPIES and warrants further study. If confirmed to be effective, it is likely to be targeted to those with approved comorbidities and those with more severe presentations.
Related blog posts: