Recently Dr. DiLorenzo gave our group a brilliant lecture. I have taken some notes and shared some slides. There may be inadvertent omissions and mistakes in my notes. Dr. DiLorenzo gave our group a lecture in 2021 as part of the William Meyers Lectureship. This talk extended those observations he conveyed at that visit (Carlo DiLorenzo: Lessons Learnt Over 30 Years). I highly recommend his upcoming NED talk at NASPGHAN.
Key points (intermixed with slides):
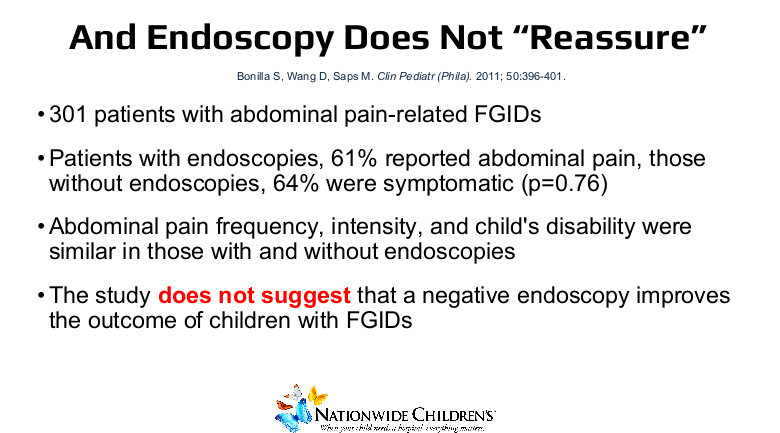
- Diagnostic testing in the setting of DGBIs is mainly for confirmation that an adequate workup has been completed
- Schedule enough time for each patient. In evaluations of visits, one of the most negative feelings for patients is when they feel rushed
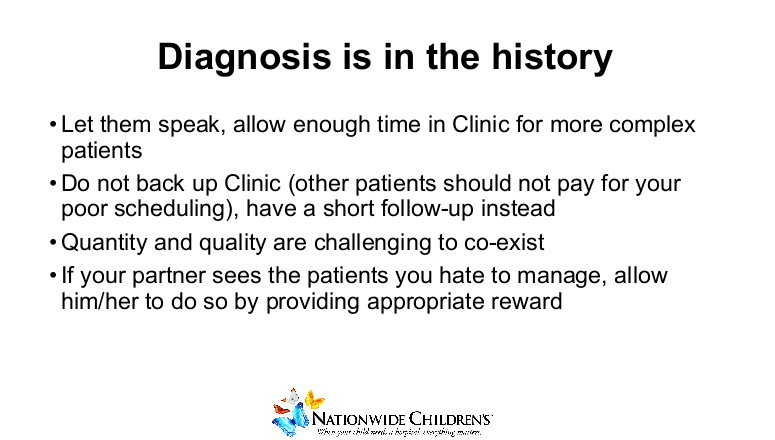
- Make sure the patient is allowed to speak. Parents may embellish (or underreport) symptoms
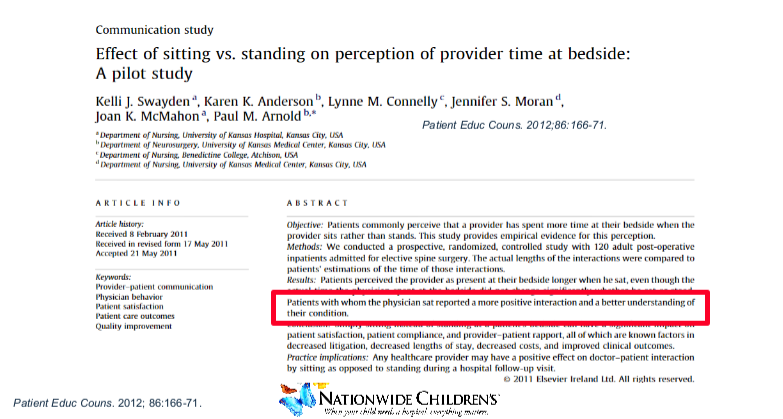
- Families feel that when clinicians are sitting down that they spend more time with them
- This extends into the hospital. A recent controlled study showed that having a chair within 3 ft of the bed increased the likelihood that physicians would sit when rounding and increased patient satisfaction (Effect of chair placement on physicians’ behavior and patients’ satisfaction: randomized deception trial. Iyer R, et al.BMJ. 2023 Dec 15;383:e076309). Study conclusion: “Chair placement is a simple, no cost, low tech intervention that increases a physician’s likelihood of sitting during a bedside consultation and resulted in higher patients’ scores for both satisfaction and communication.”
- Dr. DiLorenzo rarely uses computers when he is in the room with families
- Don’t belittle or get upset over an “easy” or “stupid” consult. All of us need help and hardly anyone wants to manage only highly-complex patients
- Don’t speak poorly of other physicians in front of the patient
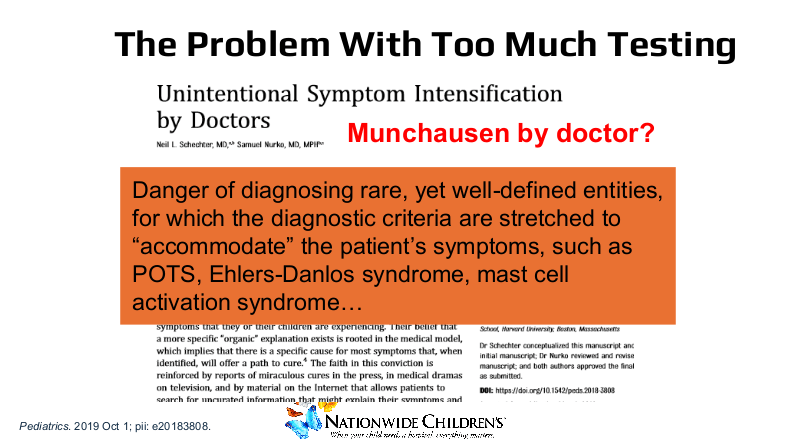
- The problem with too much testing –>it can result in ‘Munchausen by Doctor’ and the discovery of incidental problems (that may not necessitate treatment). Further testing has been associated with intensification of symptoms
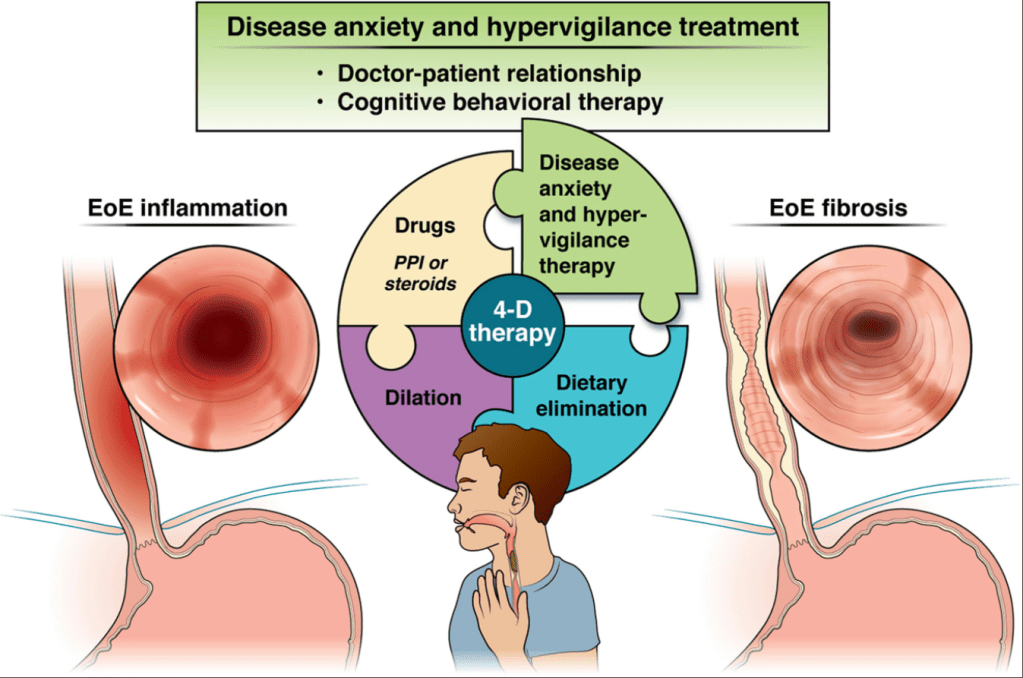
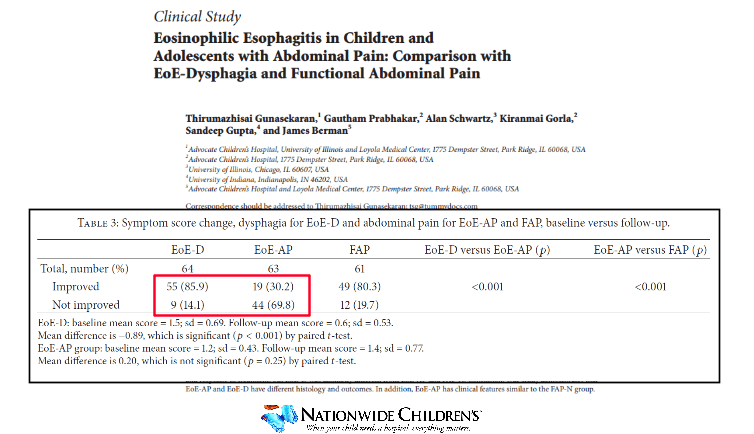
- Identification of eosinophilic esophagitis is not helpful in resolving stomach pain

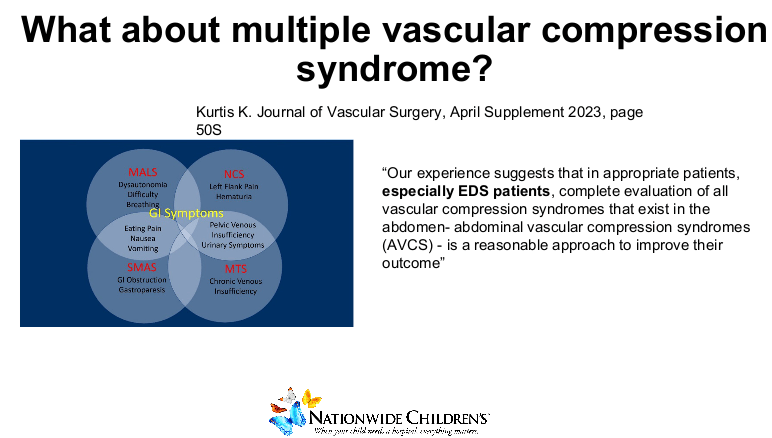
- Newest “epidemics” associated with stomach pains include alpha gal and multiple vascular compression syndrome
- While unusual disorders can occur, Dr. DiLorenzo mainly looks for unusual diagnoses when patients have unusual symptoms (like weight loss, pain with exercise)
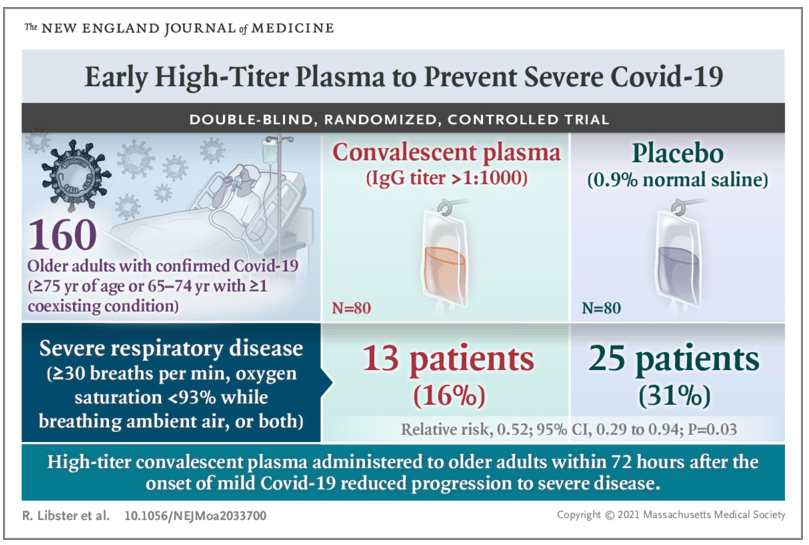
- While guidelines often emphasize the use of treatments based on double-blind, placebo-controlled (DBPC) studies, “there has never been a DBPC for the effectiveness of a parachute.” Some treatments are worthwhile even in the absence of DBPC studies
- Many of the medicines used for DGBIs and related symptoms have approval for other uses
- Fundoplication which was commonplace is used rarely these days. Yet, it is still a good treatment for reflux
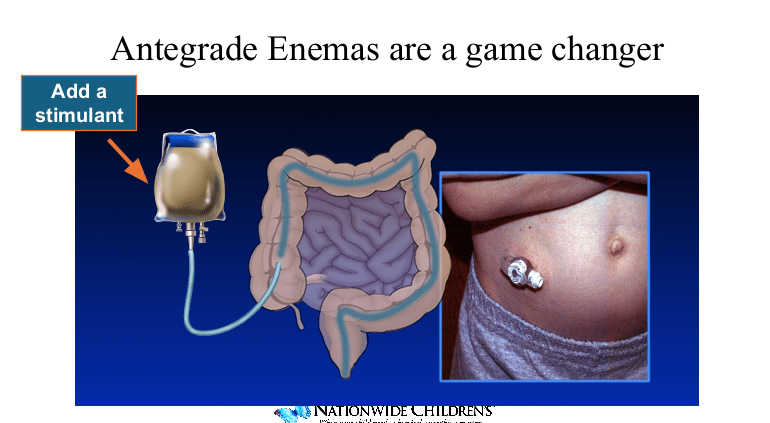
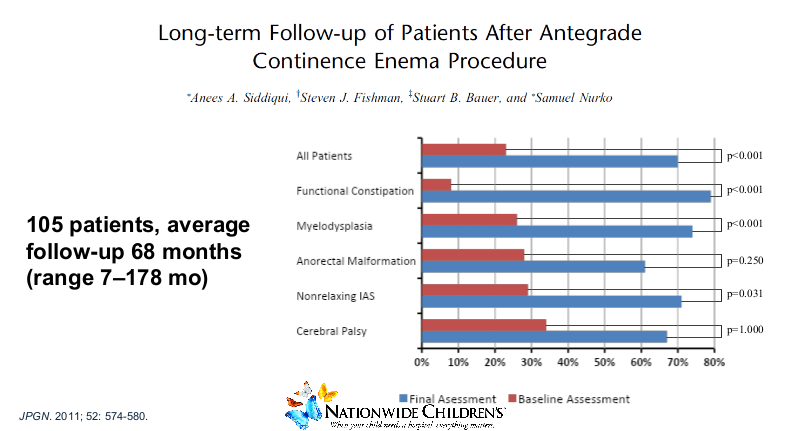
- Antegrade enemas can be very effective for constipation
- “All patients with chronic pseudo-obstruction necessitating parenteral nutrition should have a G-tube and an ileostomy.” It may help them come off parenteral nutrition
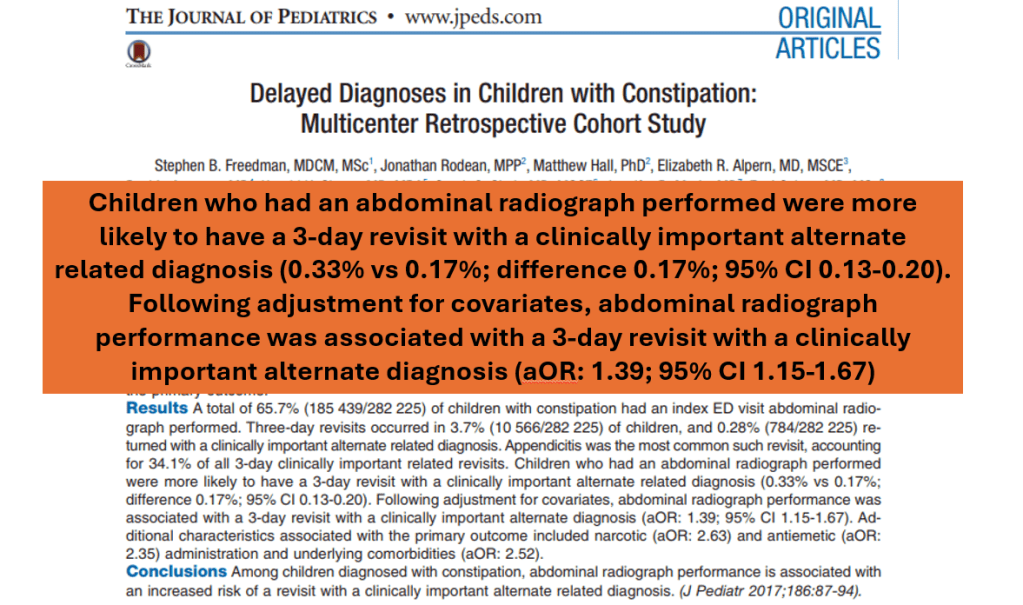
- Don’t order AXR to diagnose constipation. AXRs ordered in ER to diagnose constipation are associated with a slightly higher likelihood of a missed diagnosis.
- Though, “no need to be holier than the pope.” Using AXR in specific circumstances can be helpful with treatment (like determining success of a cleanout)
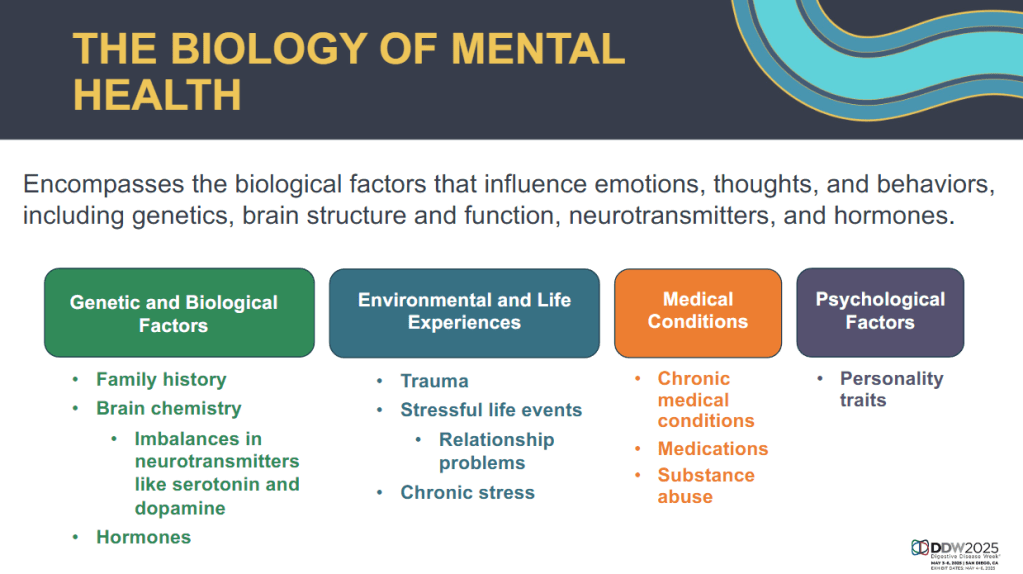
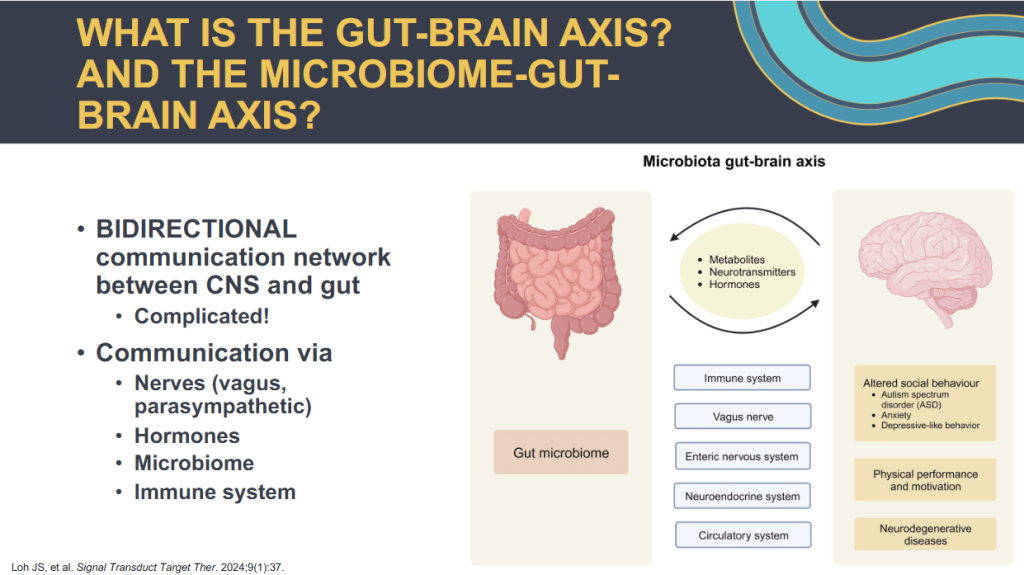
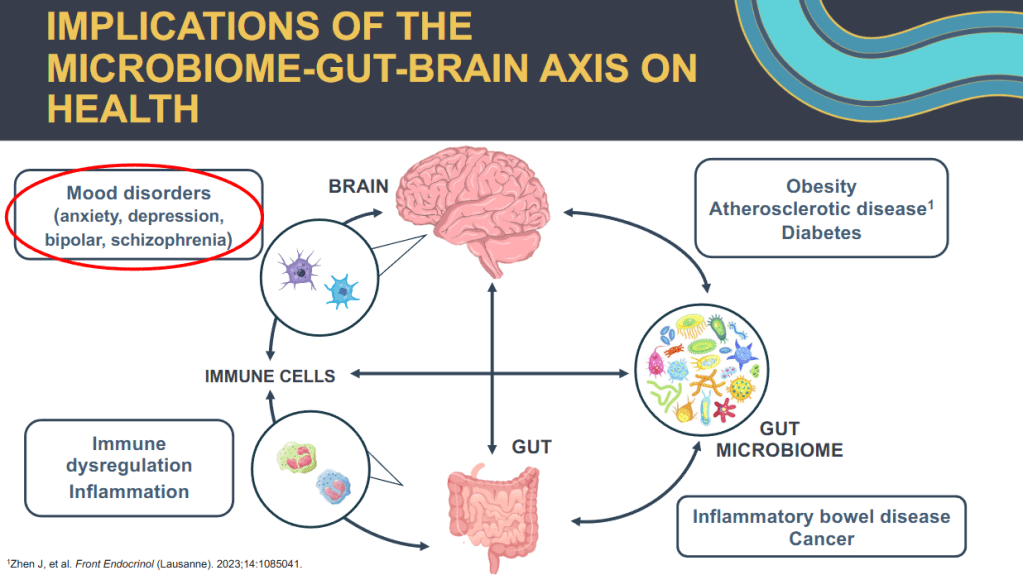
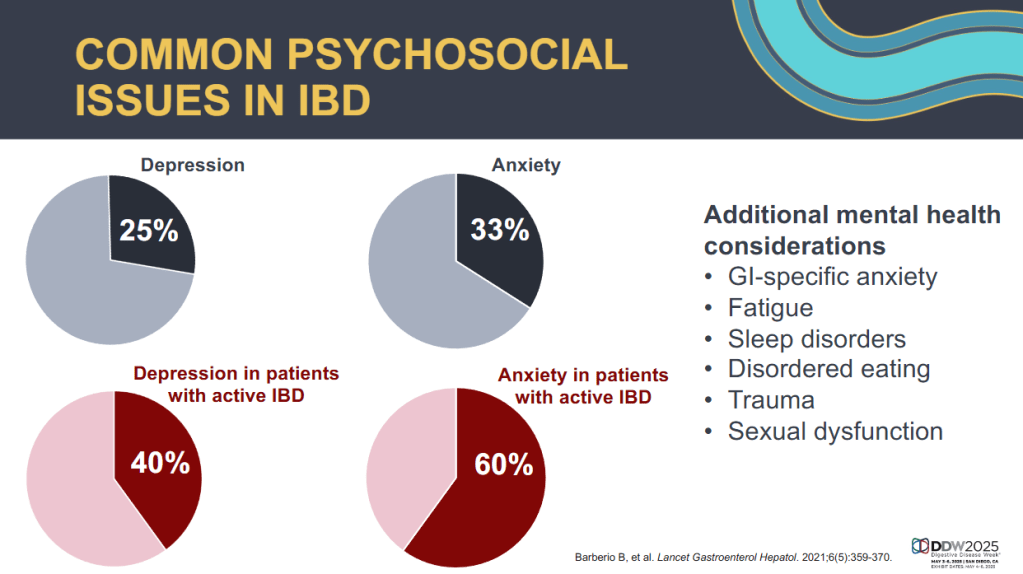
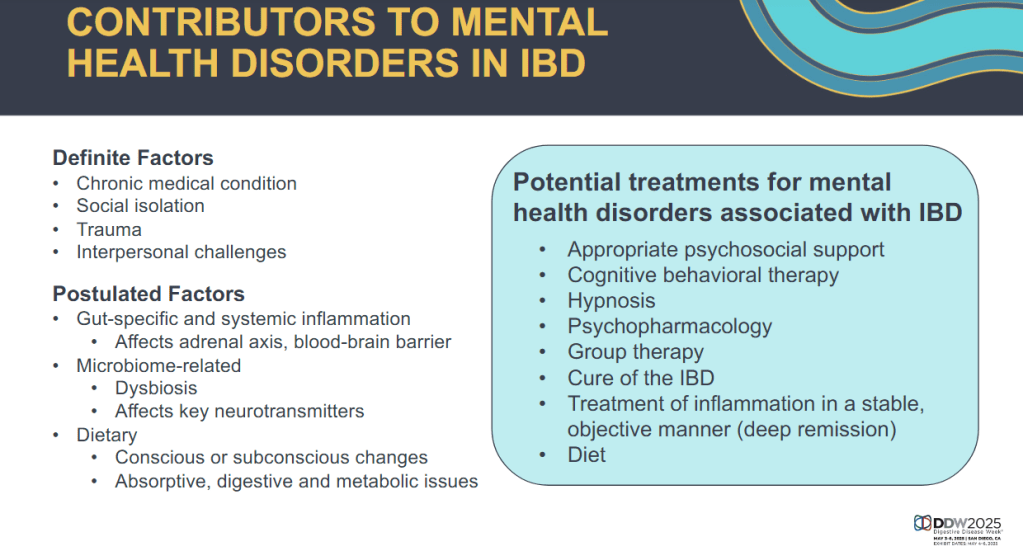
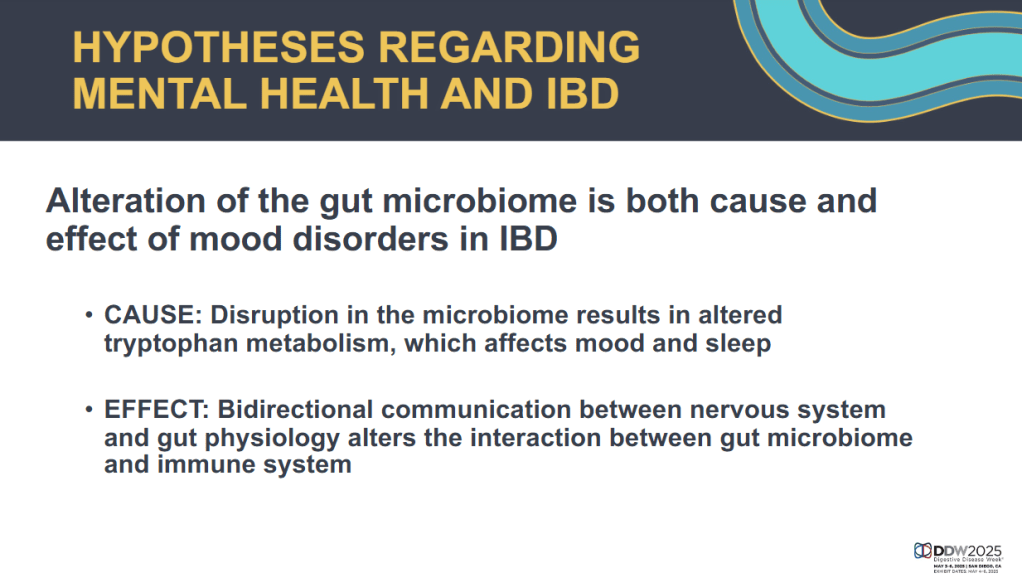
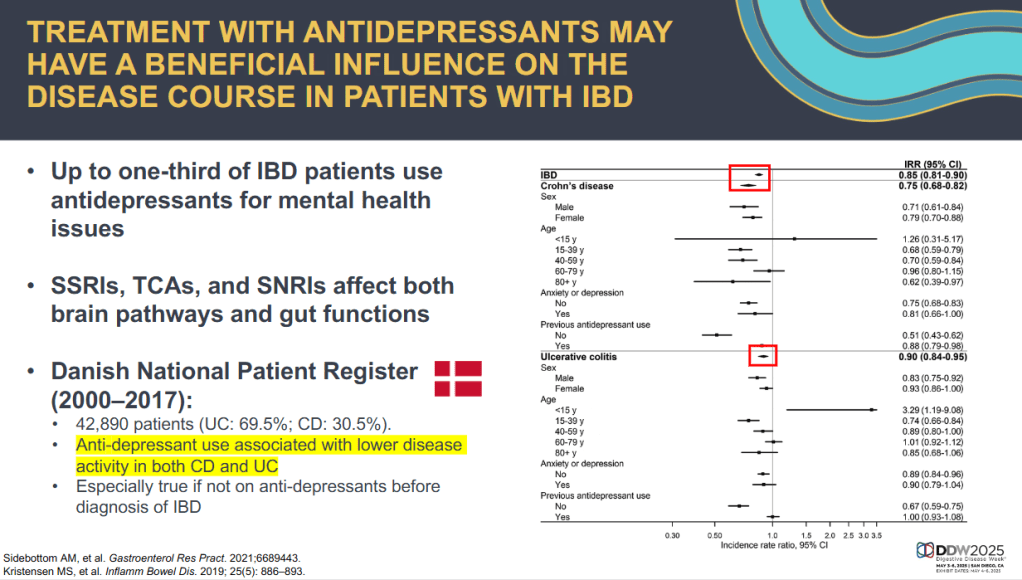
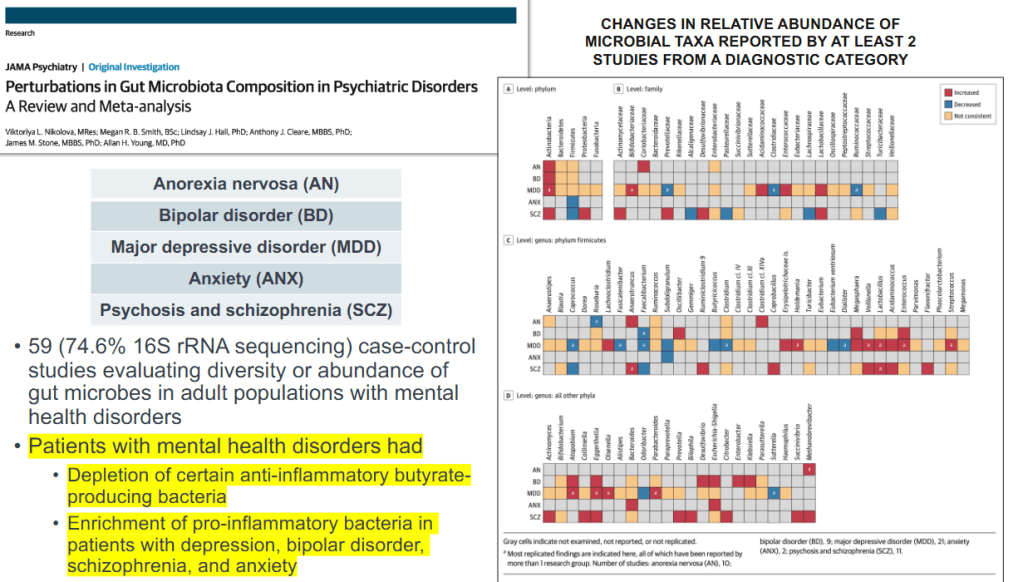
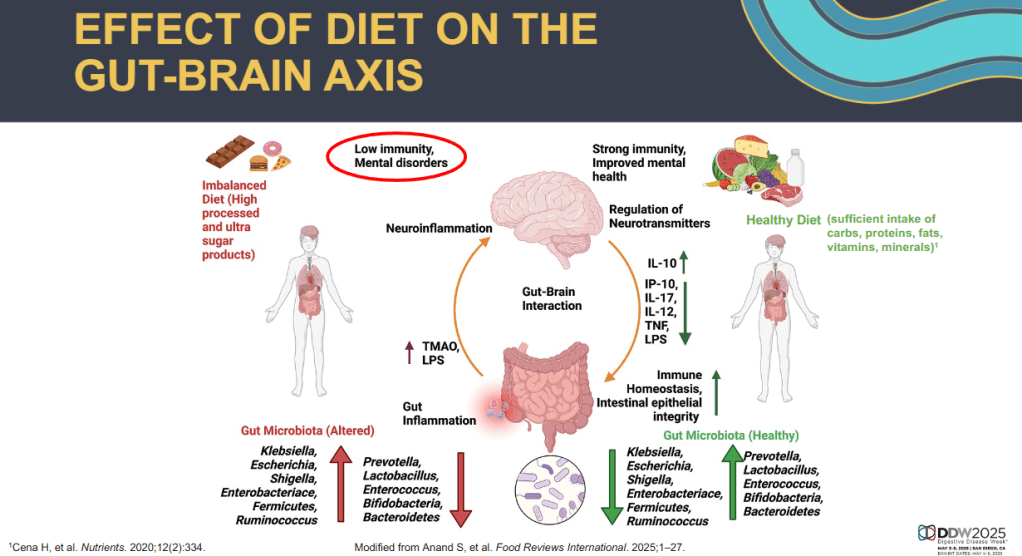
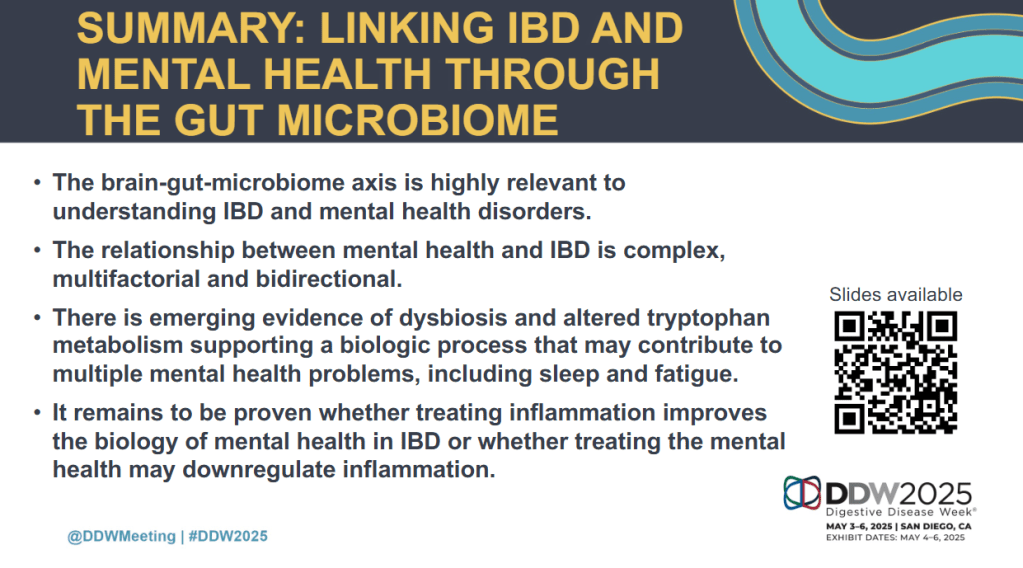
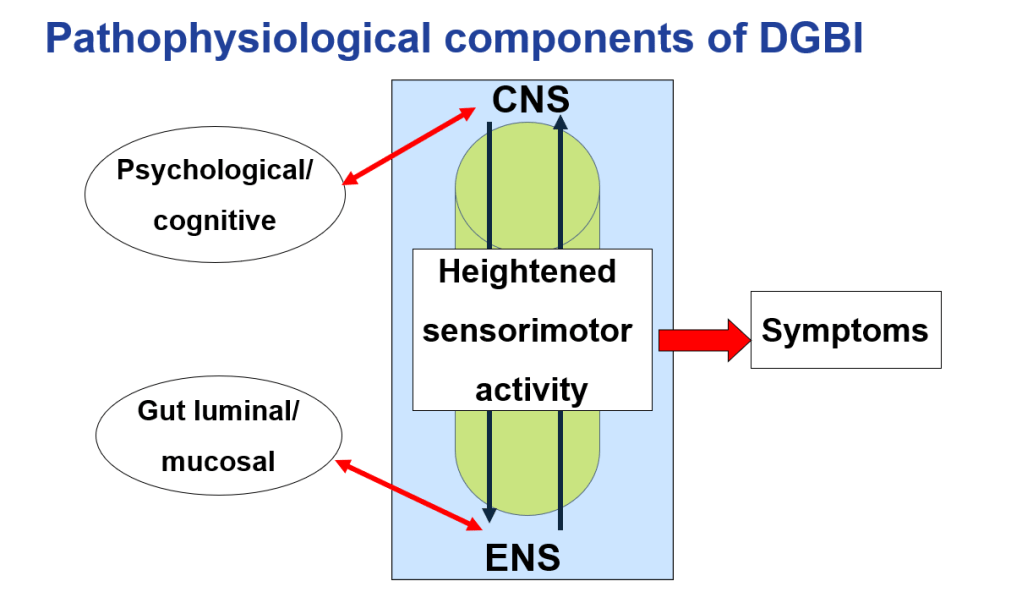
- Treating the Brain is important in patients with DGBIs
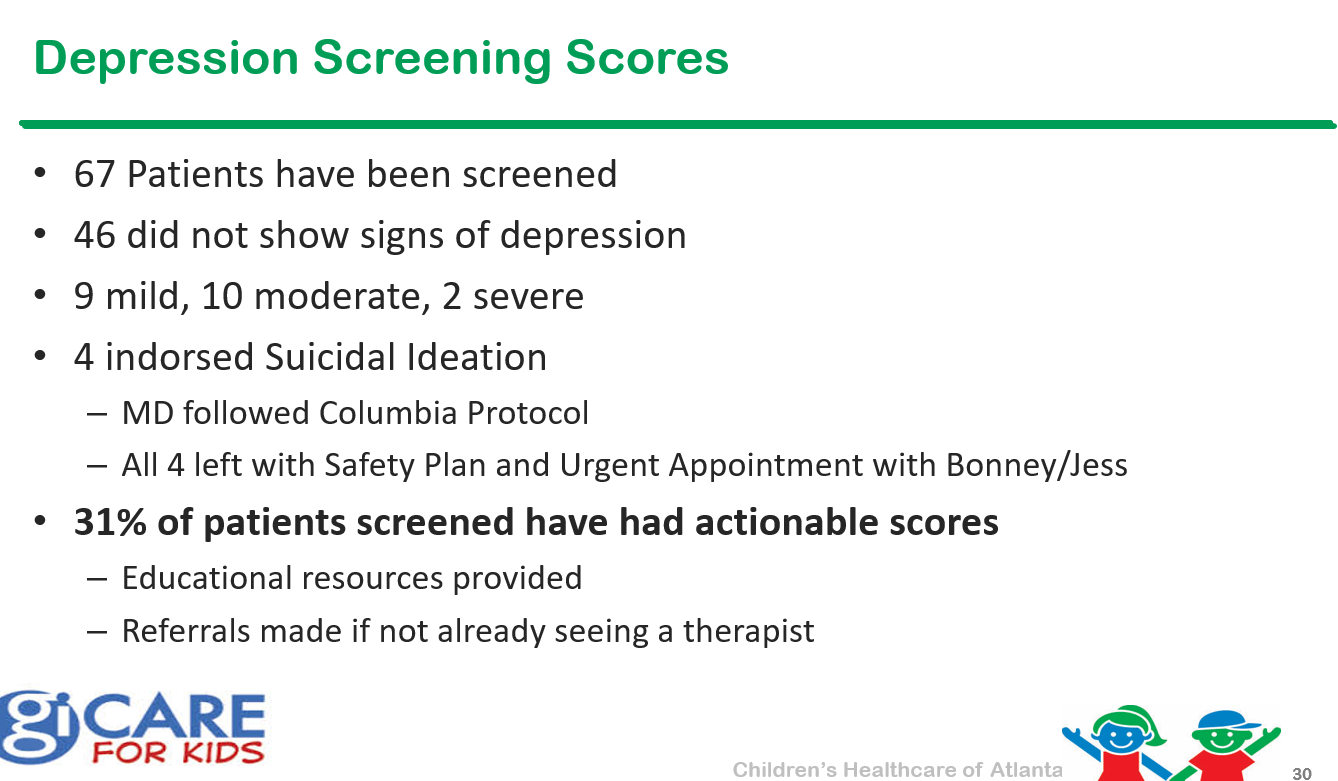
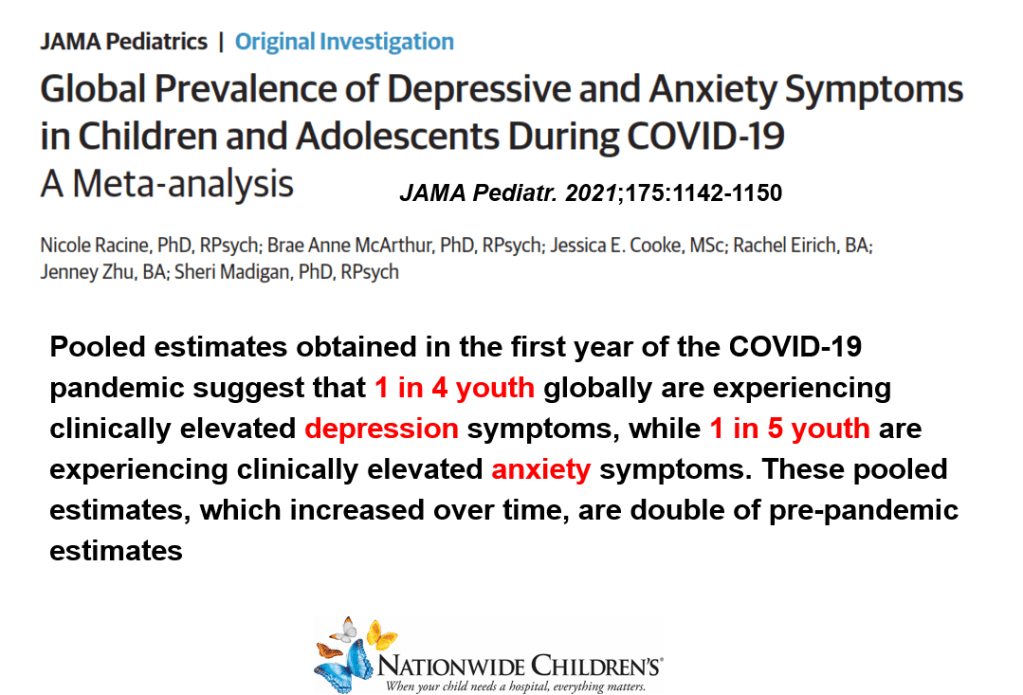
- Anxiety, which is increased in patients with DGBIs, has reached epidemic levels
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition