L Beidermann et al. Nutrients. 2024;16(23):4197. Open Access! Efficacy and Safety of Anthocyanin-Rich Extract in Patients with Ulcerative Colitis: A Randomized Controlled Trial
First of all: Bilberries are similar to blueberries, but have red inner flesh rather than white flesh.
Background: The authors note that some small studies have shown that anthocyanin-rich extract (ACRE), the bioactive ingredient of bilberries, has been effective for ulcerative colitis (UC)
“ACs have been associated with many protective biological effects, including anti-oxidative, anti-carcinogenic, antimicrobial, and anti-inflammatory properties [17,20,21]. Due to their phenolic structure, ACs exhibit an anti-oxidative capacity in vivo as they scavenge reactive oxygen species (ROS) [20,22], also a classical effect of 5-ASA [23]. After ingestion, ACs largely bypass absorption in the upper gastrointestinal tract, reaching the colon intact, where they are metabolized by microbiota through deglycosylation and further degraded into vanillic, protocatechuic, p-coumaric, gallic, and syringic acids (i.e., phenolic acids) [24]. ACs interrupt the pro-inflammatory signaling and are inhibitors of 5-lipoxygenase, a key enzyme implicated in the arachidonic acid pathway for the biosynthesis of active leukotrienes.”
Methods: A multi-center, randomized, placebo-controlled, double-blind study with a parallel group was conducted. Due to COVID-19’s effect on study enrollment, only 34 patients were randomized and only Eighteen ACRE and eight placebo patients could be analyzed (per protocol set)
Key finding:
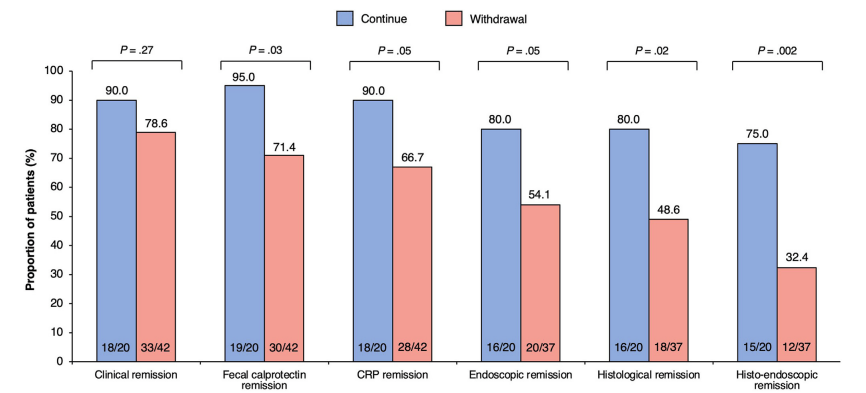
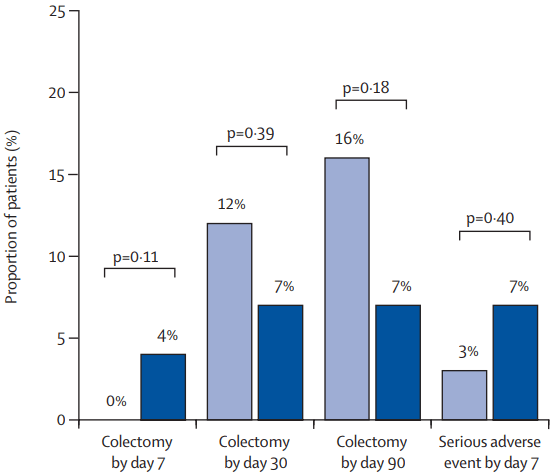
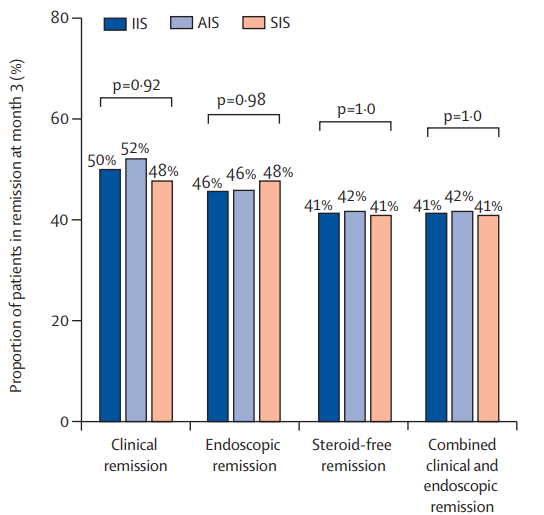
- Half (9/18) of ACRE patients and 3/8 of placebo patients responded clinically (p = 0.278). An improvement in the Mayo score was observed in the ACRE arm (77.8% vs. 62.5% placebo).
- Fecal calprotectin (FC) dropped from 1049 ± 1139 to 557 ± 756 μg/g for ACRE but not for the placebo group (947 ± 1039 to 1040 ± 1179; p = 0.035).
The authors state that the placebo group had an unusually high response and that improved FC with ACRE patients indicates efficacy in UC.


My take: This is a negative study (despite the secondary finding of improved FC at some timepoints). Importantly, the study did not demonstrate any harms in the ACRE group. It did help me understand more about bilberries!
Related blog posts: