RARA Jaoudeh et al. J Pediatr Gastroenterol Nutr. 2025;80:14–24; Pharmacological management of pediatric metabolic dysfunction-associated steatotic liver disease
Key points:
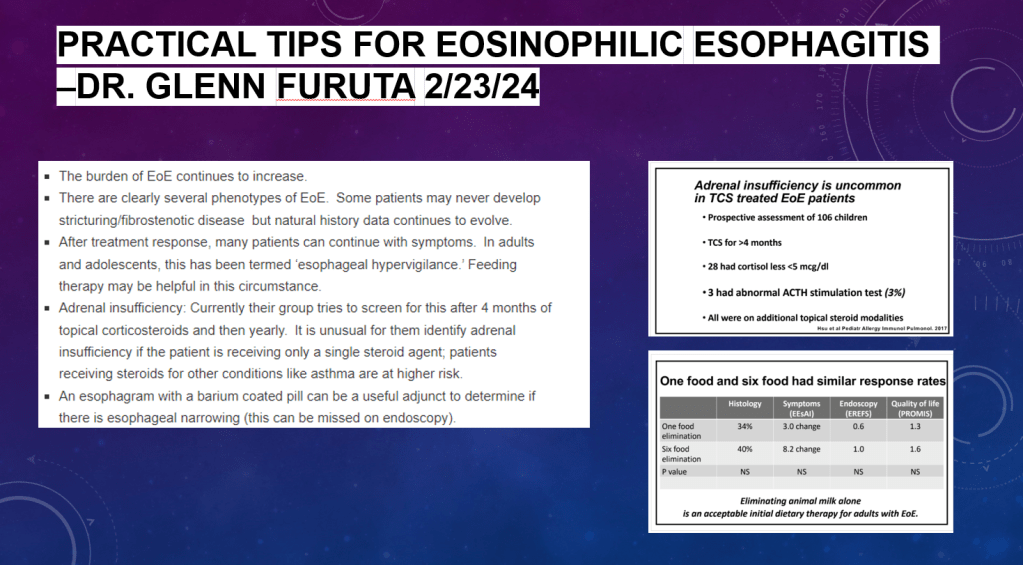
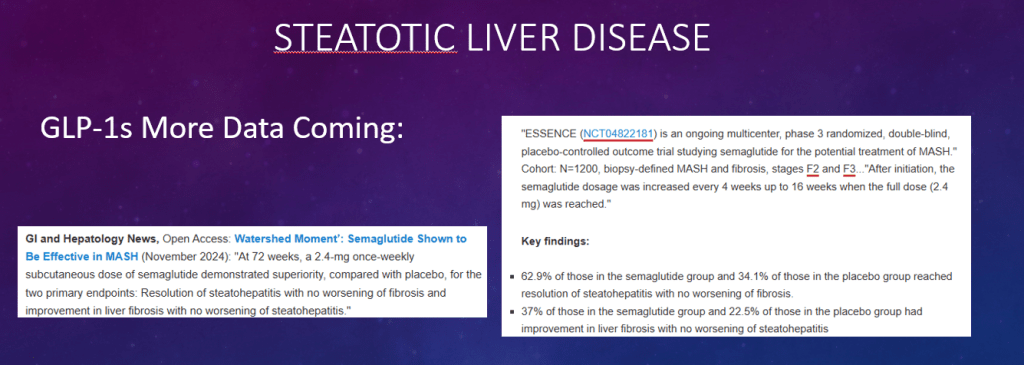
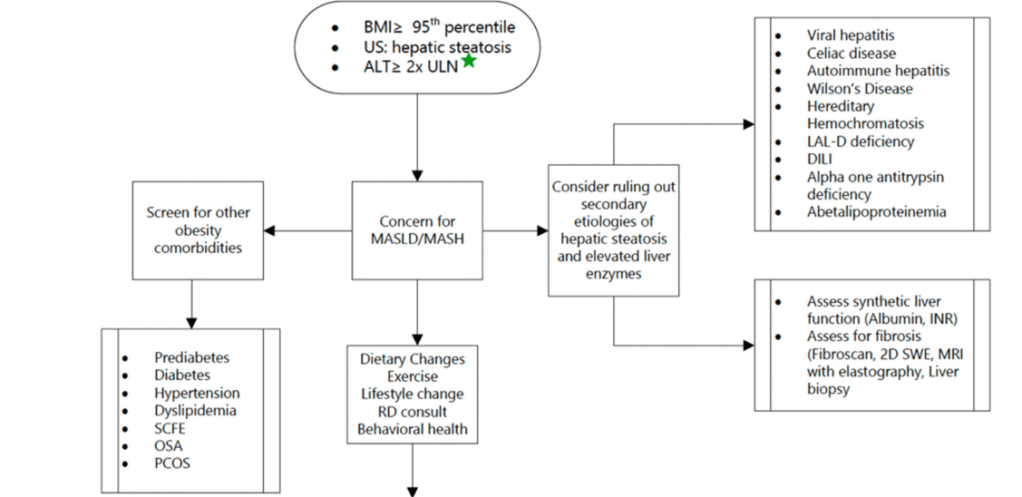
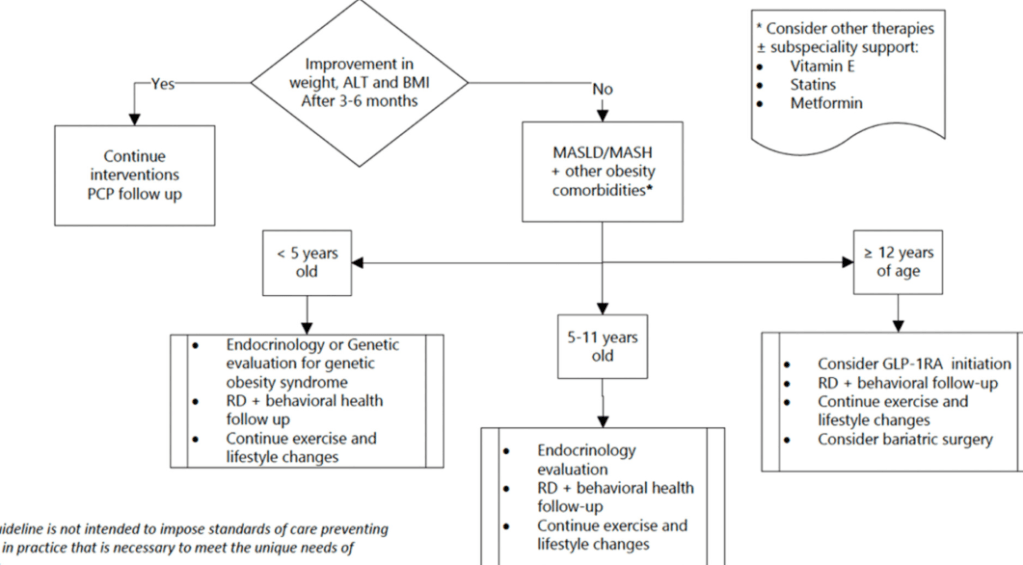
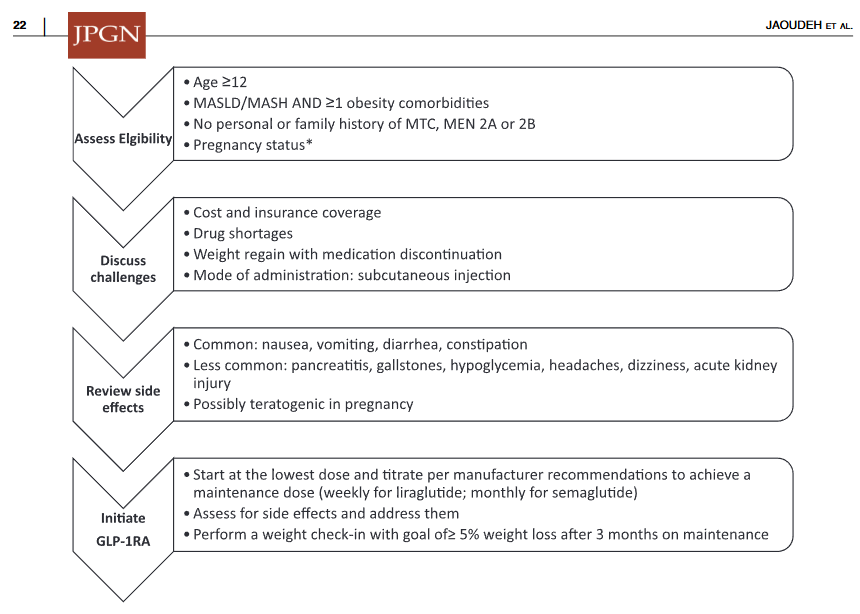
- Glucagon-like peptide-1 receptor agonists (GLP-1RAs) have demonstrated efficacy against adult MASLD. “In patients ≥12 years of age with obesity (BMI ≥ 95th percentile), we recommend the use of GLP-1RA—along with dietary and lifestyle modifications—in those who have MASLD or MASH, and 1 additional metabolic comorbidity (hypertension, prediabetes, polycystic ovary syndrome, dyslipidemia, and obstructive sleep apnea) (Figures 1 and 2). Treatment with these agents should only be initiated after other causes of hepatic steatosis are ruled out.”
- “GLP-1RA are effective in treating pediatric obesity and have shown to decrease liver enzyme levels which is likely indicative of their effect on MASLD.”
- “It is important to note that phentermine/topiramate combination drug is approved for patients 12 years and older with obesity15 and can be used as a bridge for GLP-1RA therapy in cases where access to GLP-1RA is limited.”
- GLP-1RA Dosing regimens are provided in Table 1. For example, “Semaglutide for weight loss is initiated at 0.25 mg once weekly subcutaneously and increased every 4 weeks in a stepwise fashion up to a maximum of 2.4 mg once weekly dose. The most common side effects are nausea and/or vomiting and can be worse the first few days a after dose increase. It is acceptable to delay dose escalation or reduce the target dose based on patient tolerance. Medication therapy should be evaluated for effectiveness after 12 weeks on a maximally tolerated dose.” And, “Liraglutide for weight loss is initiated at 0.6 mg daily subcutaneously and increased weekly in 0.6 mg increments up to a maximum 3 mg daily dose.”
- Adverse effects: “Both liraglutide and semaglutide have been associated with thyroid C-cell tumors in animal studies37 and are contraindicated in patients with a personal or familial history of multiple endocrine neoplasia 2A and 2B and medullary thyroid carcinoma. Patients should be educated on symptoms of thyroid tumors—lump in the neck, difficulty breathing or swallowing, or persistent hoarseness—and treatment should be discontinued if these occur.37 GLP-1RA also increase the risk of pancreatitis and gallbladder disease especially with rapid weight loss.37 Liraglutide is contraindicated in pregnancy due to potential embryo-fetal defects shown in animal studies, and semaglutide should be discontinued if pregnancy occurs.10, 37“
Useful algorithm:
My take: GLP-RAs are likely to be used increasingly in adolescents with MASLD despite issues with insurance/affordability and need for chronic treatment. This is a helpful review.
Related blog posts:
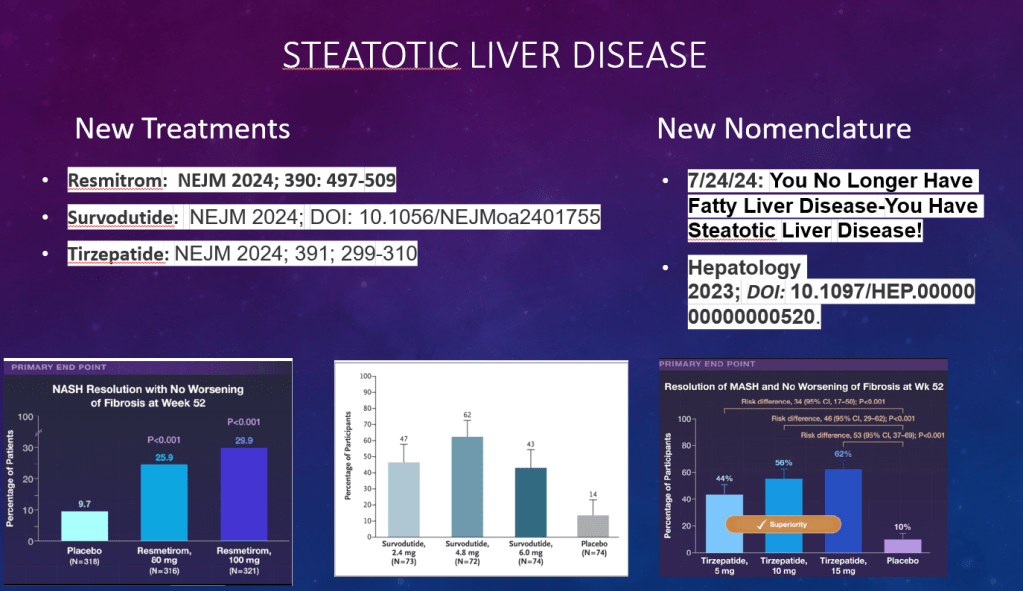
- You No Longer Have Fatty Liver Disease-You Have Steatotic Liver Disease!
- AASLD Practice Changes for Metabolic Liver Disease in 2024
- Semaglutide in Adolescent Obesity
- Survodutide, Dual Glucagon Receptor/GLP-1 Receptor Agonist, for MASH (Phase II Trial)
- Tirzepatide for Metabolic Dysfunction–Associated Steatohepatitis (MASH) & Uptick in GLP1 Use
- Pharmacotherapy for Obesity
- Fibrosis and Steatotic Liver Disease -Who Needs to be Followed by Hepatology?
- Prevalence of Steatotic Liver Disease in U.S. And Risk of Complications
- Three-fer on Steatotic Liver Disease
- Bad Fatty Liver Disease Can Get Worse Quickly
- Semaglutide Keeps Weight Off at Four Year Mark
- How Many Kids Would Be Good Candidates for Bariatric Surgery?
- Fatty Liver Disease AASLD Practice Guidance 2023

Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.