A recent study (F Fernandez-Banares et al. Am J Gastroenterol 2021; 116: 1036-1043. Persistent Villous Atrophy in De Novo Adult Patients With Celiac Disease and Strict Control of Gluten-Free Diet Adherence: A Multicenter Prospective Study (CADER Study) shows that there is a high likelihood of persistent villous atrophy among adults with celiac disease (CD) despite adherence with a gluten-free diet (GFD). Thanks to Ben Gold for showing me this paper.
Key findings:
- Among 76 patients (median age 36.5 years) who were prospectively followed for 2 years, persistent villous atrophy was observed in 40 (53%). In this group, 72.5% were asymptomatic (based on Likert scales) and 75% had negative serology
- Detectable fecal gluten immunogenic peptides (f-GIPs) were present in at least one sample in 69% of patients. (Two samples obtained at f/u visits which were ~every 6 months during study)
- Excellent or good adherence to GFD was demonstrated in 68.4% of patients based on dietetic evaluations. Only 6 (8%) were clearly nonadherent
- “There were no significant differences in the rate of clinical and serological remission between patients with villous atrophy and those with mucosal recovery”
- The authors did not find potentially modifiable predictive factors
Discussion:
- The authors note that serology is “not useful for monitoring patients on a GFD.” Anti-TTG2 and EMA, in a recent meta-analysis, had a pooled sensitivity of around 50%.
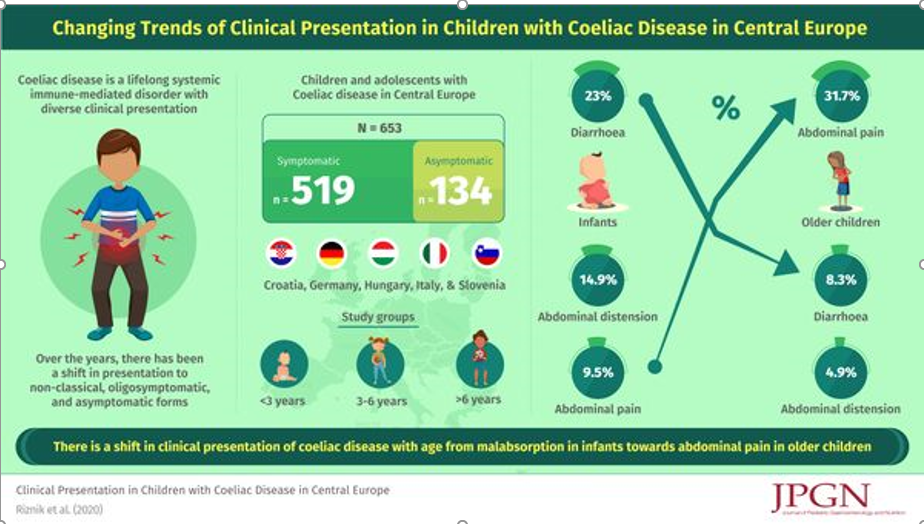
- “Adults are significantly less likely than children to normalize their duodenal histology.”
Editorial:
- The associated editorial by Rej et al (pg 946-948) outline a personalized approach for dealing with persistent villous atrophy:
- In those with persistent symptoms/positive GIPs/elevated serology/micronutrient deficiency, the first step is careful dietetic assessment. After this, endoscopy could be considered to confirm presence or absence of mucosal healing.
- In those with no symptoms and no abnormalities, use of monitoring endoscopy needs to be weighed against the costs as well as potential complications.
- Other points in the editorial: 1. GIPs have poor concordance with mucosal healing and 2. causes of poor mucosal healing include the following: natural slow healing process, super sensitive to gluten, ongoing gluten exposure, and refractory celiac disease.
My take: This study shows that there is ongoing gluten exposure in the majority of patients even in those with excellent or good adherence to a GFD; in addition, it shows that clinical/serological markers are NOT effective in predicting mucosal healing in adults. Nevertheless, it is not clear that followup endoscopy is beneficial.
Related blog posts:
- Real-World = Partially-Treated Celiac Disease
- Is a Gluten-Free Diet Possible? DOGGIE BAG Study
- #NASPGHAN19 Postgraduate Course (part 2)
- Celiac Disease: “”80 percent of success is just showing up”
- Improving Care Process in Celiac Disease
- How Slow Do Objective Markers of Celiac Disease Improve
- How Accurate is Serology at Predicting Mucosal Healing in Pediatric Patients with Celiac Disease
Forbes (7/1/21): 99.5% Of People Killed By Covid In Last 6 Months Were Unvaccinated, Data Suggests

Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition