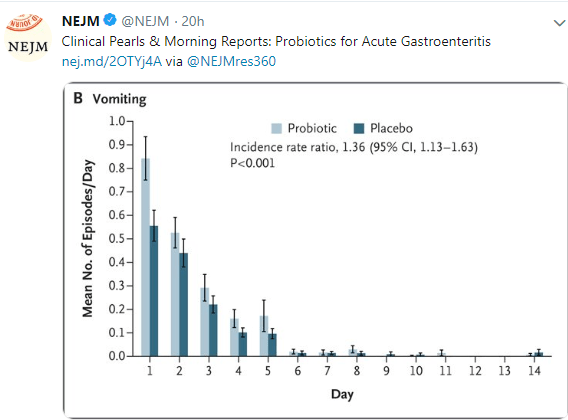
This blog post highlights a second study showing a lack of efficacy of probiotics for acute gastroenteritis. Link to 2 minute Summary: Quick Take on Probiotics for AGE
My take: While some probiotic strains have been shown to be helpful in some conditions (eg. antibiotic associated diarrhea), this study indicates that probiotics are likely ineffective in altering the course of acute gastroenteritis.
SB Freedman et al. N Engl J Med 2018; 379:2015-2026 Link to abstract: Multicenter Trial of a Combination Probiotic for Children with Gastroenteritis
Related blog posts:
- The Truth about Probiotics: Constipation Version
- Are Probiotics Effective in Changing the Microbiome?
- Lactobacillus rhamnosus GG Associated with Increased Necrotizing Enterocolitis in Observational Study
- How helpful are probiotics?
- Balanced summary of probiotics & Microbiome effects on brain
- Probiotics for Crohn’s Disease –No Beneficial Effects Noted | gutsandgrowth
- Probiotics For Fatty Liver Disease | gutsandgrowth
- “Low quality of evidence; strong recommendation” for Probiotics in Gastroenteritis
- Probiotics for Colic
- Do Probiotics Really Help Crying Infants? | gutsandgrowth
- Pushback on Probiotics
- One More Day Syndrome & Necrotizing Enterocolitis | gutsandgrowth
- Probiotics, Atopy, and Asthma | gutsandgrowth