KA Madsen et al. JAMA Pediatr. Published online November 16, 2020. doi:10.1001/jamapediatrics.2020.4768.Full text link: Effect of School-Based Body Mass Index Reporting in California Public Schools
Methods: Cluster randomized clinical trial. The Fit Study (2014-2017) randomized 79 California schools (n=28 641 students) to BMI screening and reporting (group 1), BMI screening only (group 2), or control (no BMI screening or reporting [group 3]) in grades 3 to 8. The setting was California elementary and middle school
Key findings:
- Among 6534 of 16 622 students with a baseline BMI in the 85th percentile or higher (39.3%), BMI reporting had no effect on BMI z score change (−0.003; 95% CI, −0.02 to 0.01 at 1 year and 0.01; 95% CI, −0.02 to 0.03 at 2 years)
- Weight dissatisfaction increased more among students having BMI screened at school (8694 students in groups 1 and 2) than among control participants (5674 students in group 3).
My take: Tackling obesity will require a lot more than measuring BMIs. An interesting follow-up study would be to see if schools who reported BMIs were more likely to take other measures, such as providing nutritional counseling, improving school lunch selection, and providing opportunity for more activity/exercise.
Related blog posts:
- Leave Overweight Kids Alone
- Parent Fat Stigma
- “The Paramount Health Challenge for Humans in the 21st Century”
- NY Times: “Our Food is Killing Too Many of Us”
- Skinnier TVs and Heavier Kids | gutsandgrowth
- 7 Ways Parents Can Influence Risk of Obesity
- Eliminating sweetened beverages to help obesity
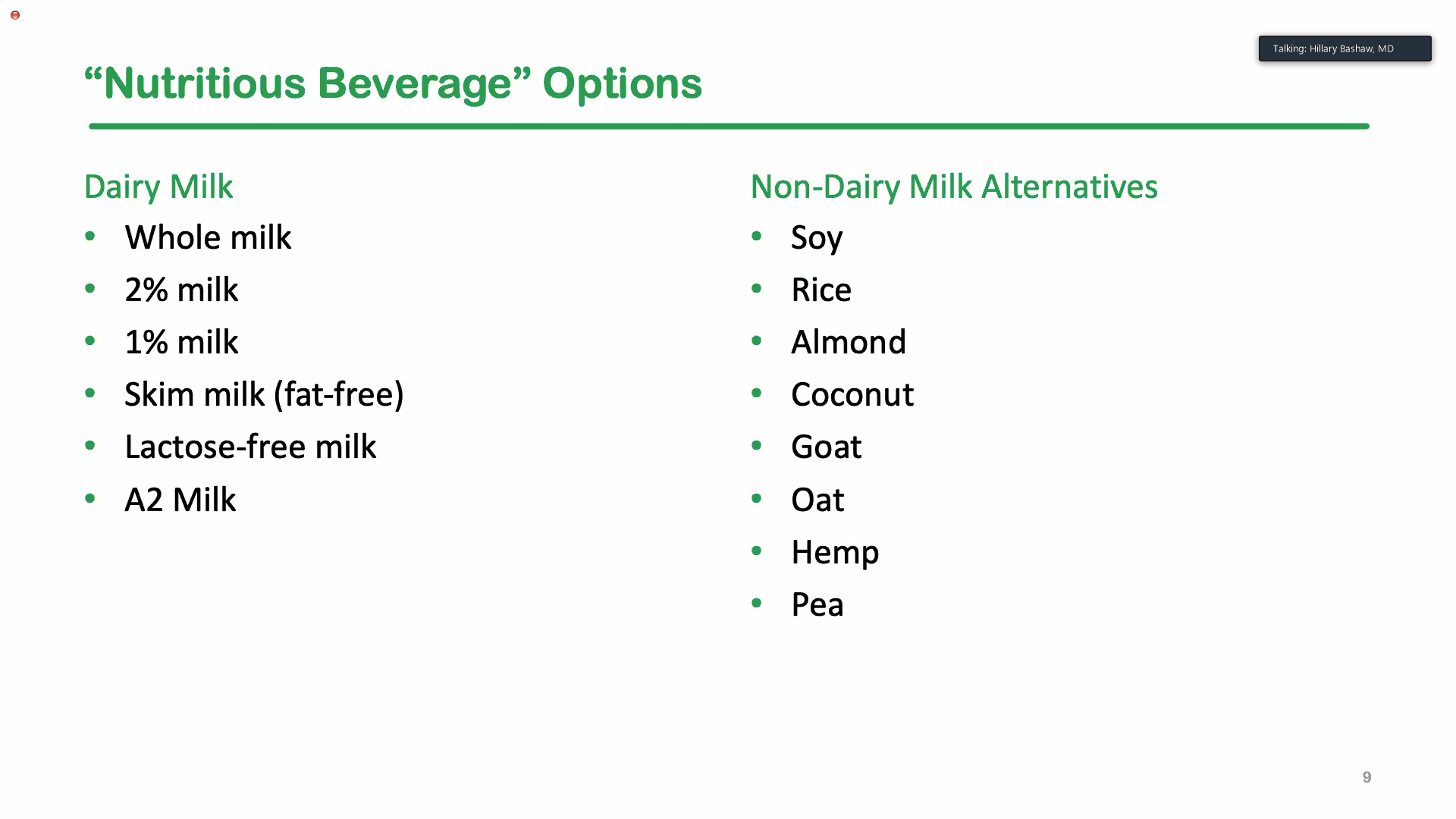
- Nutrition ‘Mythbuster’ Webinar