P Lukina et al. Clin Gastroenterol Hepatol 2025; 23: 1143-1151. The Prevalence and Rate of Undiagnosed Celiac Disease in an Adult General Population, the Trøndelag Health Study, Norway
Methods: The study used the fourth Trøndelag Health Study (HUNT4), conducted in 2017–2019, where 56,042 adult (aged >20 years) residents of Nord-Trøndelag County, Norway, participated. Serum samples from 54,505 participants were analyzed for anti-transglutaminase 2 IgA and IgG.
Key findings:
- The rate of CeD seropositivity was 2.0% (1107/54,505).
- The total biopsy-confirmed prevalence of CeD was 1.5% (853/56,042).
- The study confirmed a new CeD diagnosis after participation in HUNT4 in 470 individuals and a known CeD diagnosis before participation in HUNT4 in 383 individuals.
- The ratio of new, previously undiagnosed CeD cases (after HUNT4) to known, previously diagnosed CeD cases (before HUNT4) was 1.2:1 (470/383).
My take: This study showed that the ratio of undiagnosed cases to diagnosed case of CeD was improved from previously in Norway.
EM Hård af Segerstad, et al. Gastroenterol 2025; 168: 1185-1188. Open Access! Early Dietary Fiber Intake Reduces Celiac Disease Risk in Genetically Prone Children: Insights From the TEDDY Study
Methods: This study examined the quantity and timing of dietary fiber intake in children up to 5 years of age who were at genetic risk for celiac disease, assessing its relationship with their subsequent risk of developing the condition. The analysis included 6520 children carrying the HLA-DQ2 and/or DQ8 risk haplotypes who were prospectively followed for a total 61,669 person-years to age 13 years in The Environmental Determinants of Diabetes in the Young (TEDDY) study.
Key findings:
- Dietary fiber intake from 6 months to 3 years of age was inversely associated with the subsequent risk of celiac disease in models unadjusted for the concurrent gluten intake and to 2 years of age in models adjusted for gluten intake (Figure 1A). In contrast, no association was observed between dietary fiber intake to 4 and 5 years of age and the risk of celiac disease regardless of whether models accounted for the gluten intake.
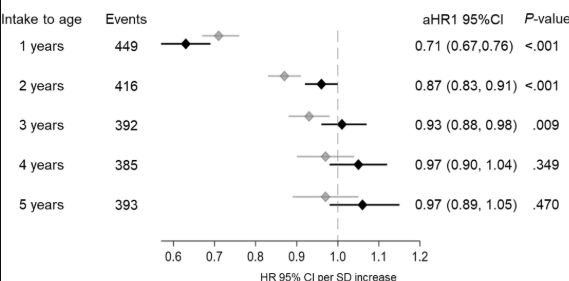
My take: Higher dietary fiber intake during the first 2 years of life was associated with a lower risk of celiac disease in children at genetic risk. Although this effect was modest, it was independent of gluten intake and other components found in fiber-rich foods in the child’s diet.
Related blog posts:
- Dr. Arun Singh: Tips and Tricks to Managing Celiac Disease
- Titers Associated with Isolated Duodenal Bulb Presentation
- What To Do For Pediatric Patients with Non-Responsive Celiac Disease
- Celiac Disease: Pro Tips (Part 1)
- Celiac Disease: Pro Tips (Part 2)
- Celiac Disease: Pro Tips (Part 3)
- Celiac Disease: Pro Tips (Part 4)
- 2023 ACG Celiac Guidelines for Adult and Children
- Taking One ‘Bite’ At A Time -For Celiac Diagnosis | gutsandgrowth
- Celiac Disease: “”80 percent of success is just showing up” | gutsandgrowth
- What To Do For Pediatric Patients with Non-Responsive Celiac Disease
- Predicting Risk of Celiac Disease in High-risk Families
- Celiac Advocacy: Food Labeling Modernization Act
- Persistent Villous Atrophy in Celiac Disease Despite a Gluten-Free Diet
- Real-World = Partially-Treated Celiac Disease
- Best Screening For Celiac At All Ages