AGA GastroNews, AGA IBS in America survey reveals IBS major burden despite advances in treatment (8/7/25):
Methods: The Harris Poll on behalf of AGA in 2024, among 2,013 U.S. adults age 18+ who have been diagnosed by a health care provider with IBS-C (1,005) or IBS-D (1,008). In addition, U.S. health care provider research was conducted online among 600 health care providers including gastroenterologists (n=200), primary care physicians (PCPs, n=200), gastroenterology nurse practitioners (NP)/physician assistants (PA) (n=100), and PCP NP/PAs (n=100)
Key findings:
- IBS symptoms interfere with patients’ productivity at work/school for nearly 11 days per month on average
- IBS symptoms disrupt personal activities eight days per month on average
- 69% say their symptoms make them feel like they’re not “normal”
- 77% avoid situations where bathroom access is limited.
- 72% find it difficult to plan activities due to unpredictable symptoms.
- 72% stay home more often because of their symptoms
My take: This sample of patients with IBS likely has more severe symptoms than a more general population of patients with IBS. Nevertheless, it highlights the impact of IBS symptoms on daily living.
Link: AGA IBS Toolkit
Related blog posts:
- Tailoring IBS Dietary Therapy Based on Proprietary IgG-Based Blood Test –Does It Work?
- Treatment Guidelines for Pediatric Irritable Bowel Syndrome
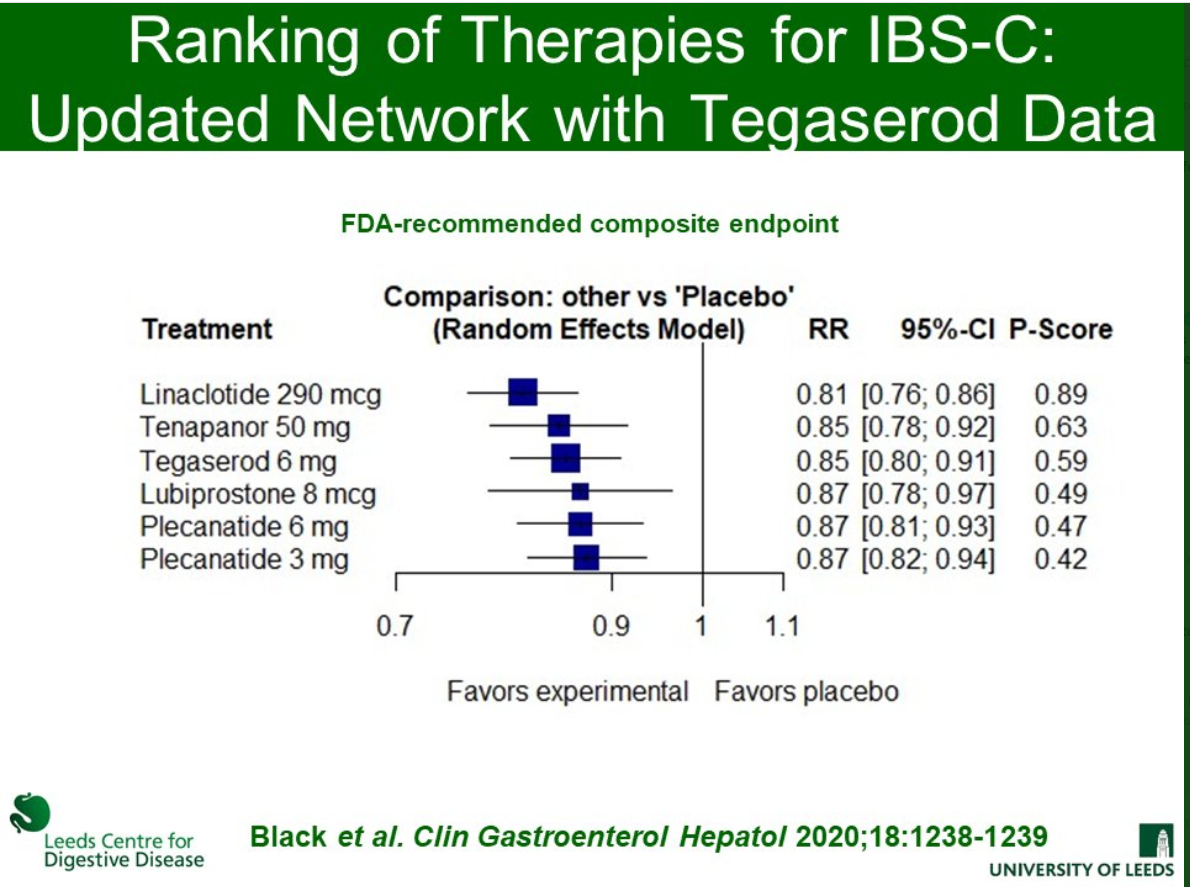
- AGA Guidelines for Pharmacologic Therapy of IBS-D and IBS-C
- Will This Abdominal Pain Last Forever? Part 3 (2024)
- Enhanced Placebo Effect For Irritable Bowel Syndrome and Functional Abdominal Pain in Adolescents
- Craig Friesen: Understanding Food Allergies and Food Intolerance in DGBIs
- Dr. Carlo DiLorenzo: Advice for Managing DGBIs (Part 1)
- Dr. Carlo DiLorenzo: Advice for Managing DGBIs (Part 2)
- Dr. Neha Santucci: Management of DGBIs in the Post-Pandemic Era (Part 1)
- Prospective Pediatric Study of the Persistence and Progression of Recurrent Abdominal Pain