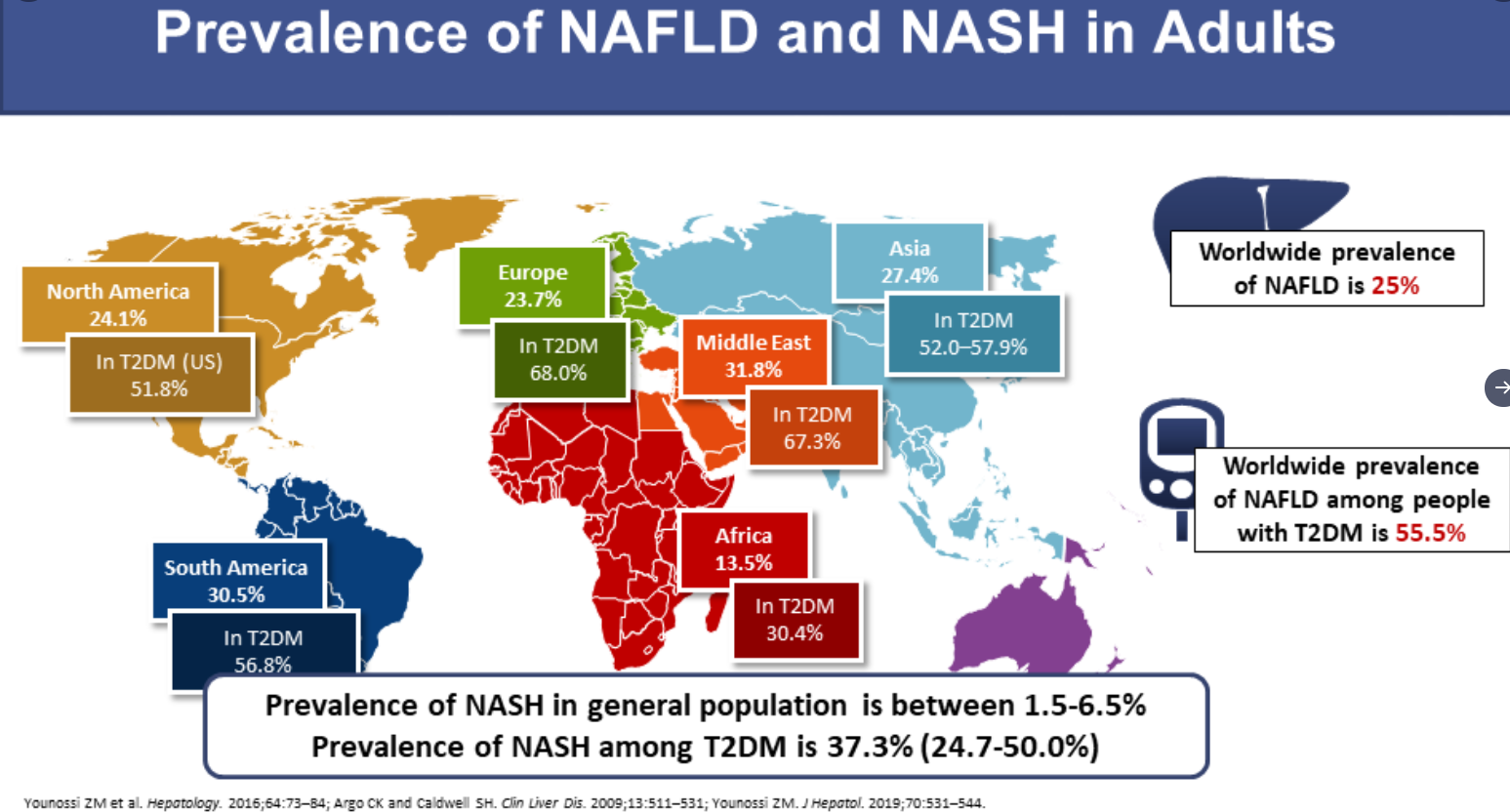
Looking for and managing hypertension has been an important component of care in children and adults with nonalcoholic fatty liver disease (NAFLD)/metabolic syndrome. In addition, hypertension is frequently associated with renal impairment.
As such, it is perhaps not surprising that in both adults and children, there is a high rate of renal impairment. The data in children is much more sparse than in adults. A recent retrospective pediatric cohort study (T Yodoshi et al. J Pediatr 2020; 222: 127-33) adds more information to this problem.
More background information:
- Chronic kidney disease is highly prevalent in adults with NAFLD: 20-55% (J Hepatol 2020; 72: 785-801; Am J Kidney Dis 2014; 64: 638-52)
- NAFLD is currently the leading indication for concurrent liver and kidney transplantation
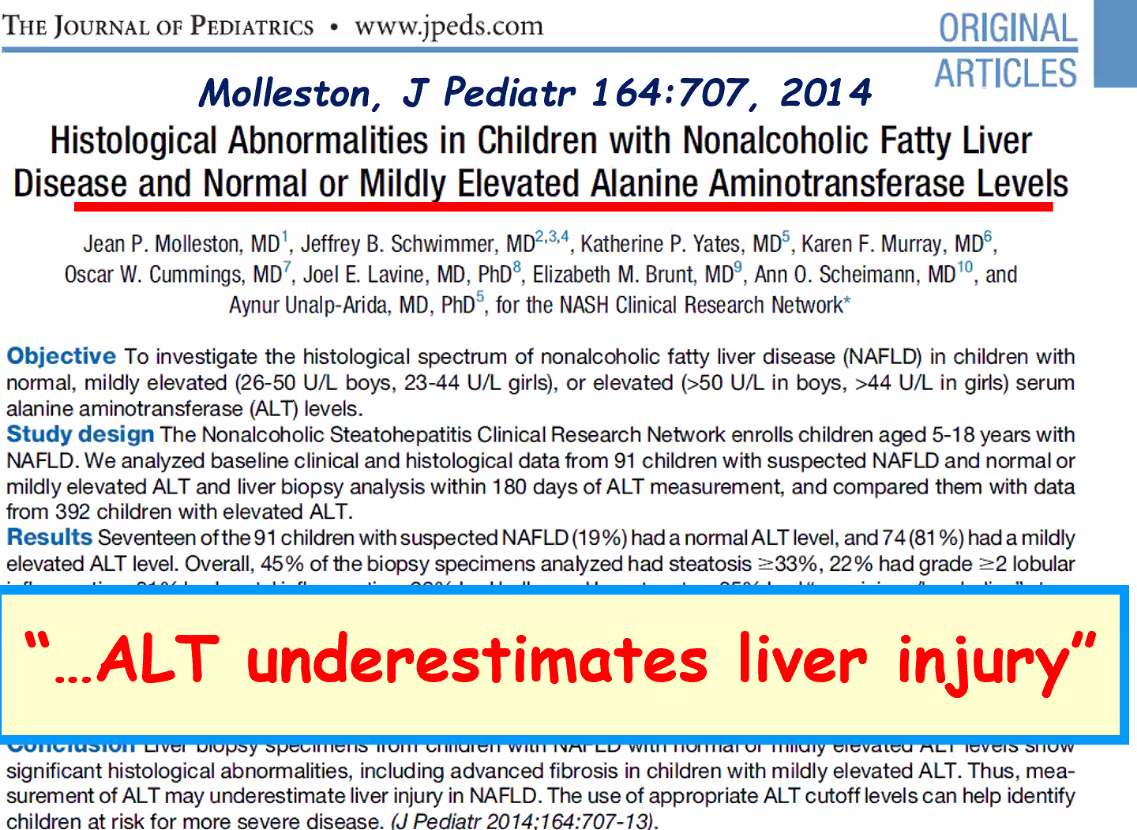
- In adults, the severity of NAFLD histology is associated with renal impairment
- The first stage of renal impairment is glomerular hyperfiltration. This is hypothesized to be a precursor of intraglomerular hypertension which leads to albuminuria and glomerular filtration rate (GFR) decline/progressive renal dysfunction
- Early intervention in high risk patients with angiotensin receptor inhibitors may prevent or delay progressive renal disease
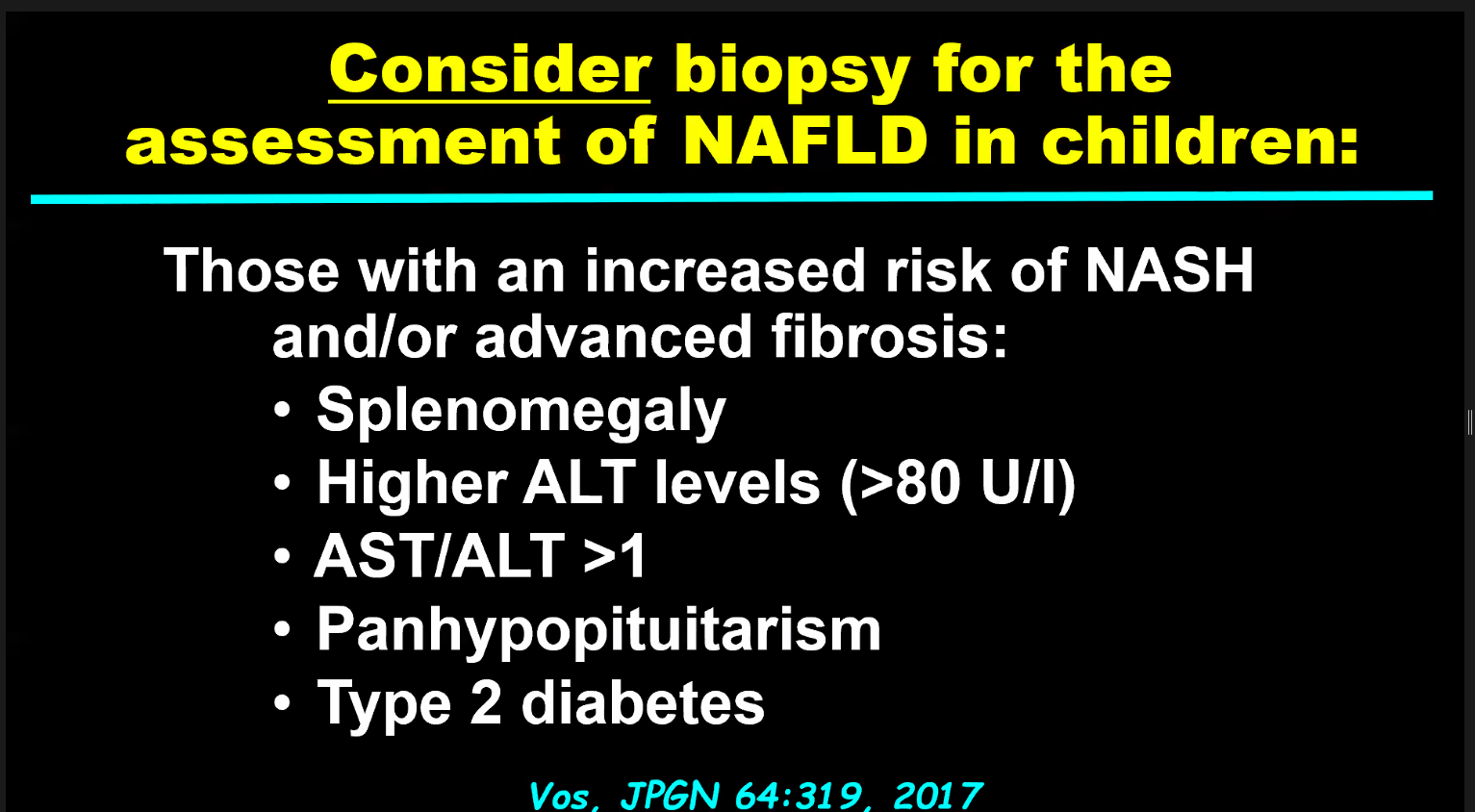
Key findings in 179 patients with biopsy-confirmed NAFLD:
- 82% non-Hispanic, median age 14 yrs
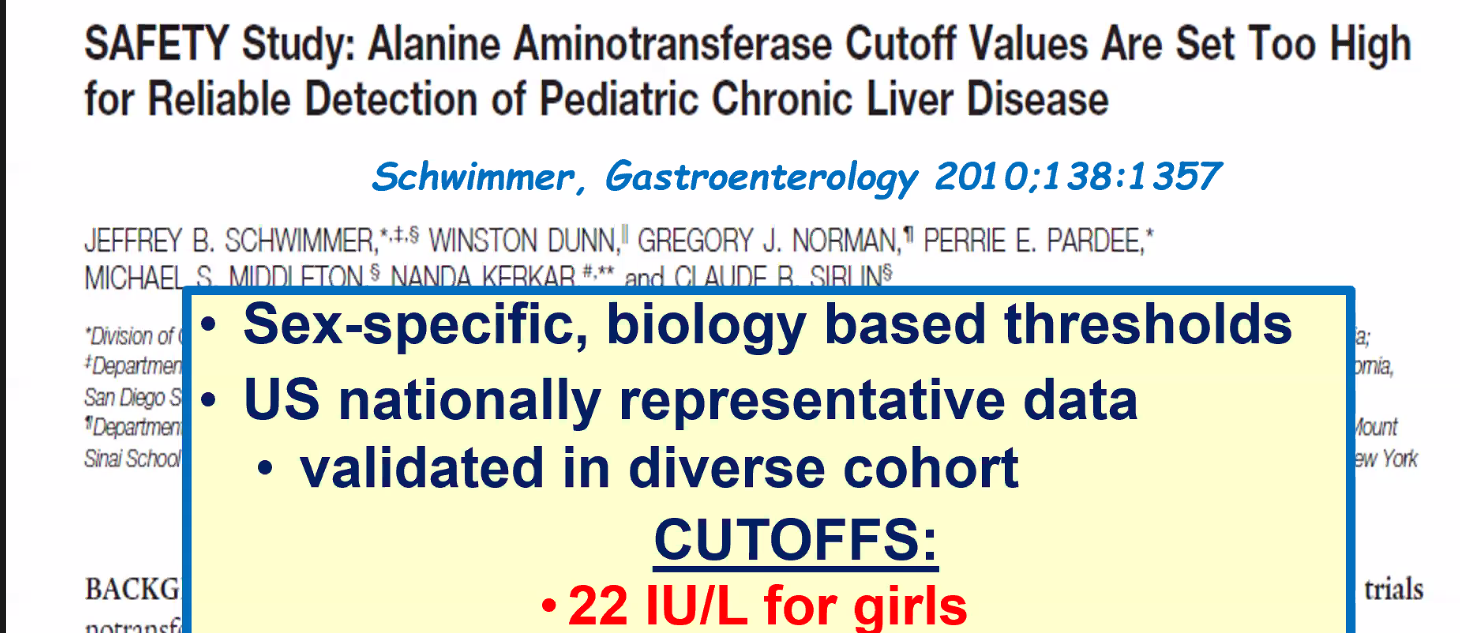
- 36 (20%) had glomerular hyperfiltration and 26 (15%) had low GFR (w/in 3 months of liver biopsy) based on Schwartz equation
- Hyperfiltration was independently associated with higher NAFLD activity score (aOR 2.96)
Discussion:
- Mechanism: The authors speculate that “it is possible that they [renal and liver disease] are both the end result of the same ‘hit.’ The renin-angiotensin system may play a key role….Notably, there is an ongoing…clinical trial investigating an ATI receptor blocker, losartan, for the treatment of NAFLD in children.” Other potential contributors include fructose and insulin resistance.
- Limitations: This single center biopsy-confirmed population may not be representative of most children with NAFLD. Also, as this was a retrospective study, more precise measures of renal function were not available.
My take: This study confirms a high rate of renal dysfunction (35%) in children with NAFLD. As such:
- Children with NAFLD need to have their blood pressure monitored
- Clinicians should have a low threshold for nephrology referral if suspected renal impairment.
NEJM Recovery Collaborative Group: July 17, 2020
DOI: 10.1056/NEJMoa2021436: Full Link: Dexamethasone in Hospitalized Patients with Covid-19 — Preliminary Report
Form NEJM Journal blog:
In the open-label RECOVERY trial, some 2100 U.K. patients hospitalized with COVID-19 were randomized to usual care plus oral or intravenous dexamethasone (6 mg once daily for up to 10 days), and 4300 were randomized to usual care alone.
Among patients on invasive mechanical support at the time of randomization, the mortality rate within 28 days was significantly lower with dexamethasone than with usual care alone (29% vs. 41%). A benefit was also seen among those on oxygen without invasive ventilation (23% vs. 26%). However, among patients not receiving respiratory support, mortality rates did not differ significantly between treatment groups.