A recent study (NE Newman, KL Williams, BJ Zikmunde-Fisher, J Adler. JPGN 2020;70: e33-36) highlights work to communicate the benefits and risks of the treatment for inflammatory bowel disease (IBD) along with the risks of untreated IBD. “We developed a simple video aid to illustrate competing risks associated with medications and underling disease in context of inflammatory bowel disease…Those who viewed the video aid had more realistic perceptions than those who did not view it.”
Here is a link to the ~13 minute online video: IBD: Risk of Disease and Treatments
Overall, the presentation is very helpful and thoughtful. I think this would be an excellent overview for families. For practitioners, a few points that could benefit from some nuance are noted below some screenshots. It is worth stating that the authors had started this project a few years ago and some of the points below are related to more information that has emerged.

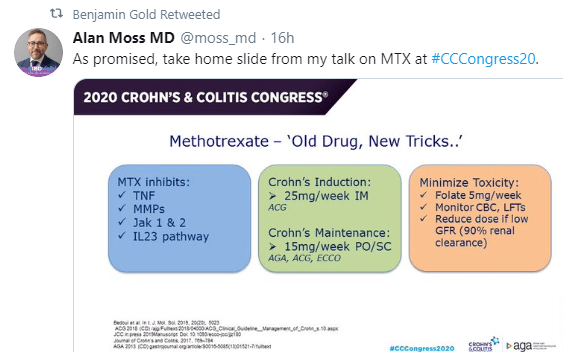
In the section of treatment benefits (above), the presentation suggests that thiopurines (azathioprine, 6-mercaptopurine) and methotrexate both are effective in about 50%; this is probably an overestimate; in addition, methotrexate as monotherapy is definitely less effective (if effective at all) for ulcerative colitis . Also, it would be worthwhile to indicate that anti-TNF monotherapy with therapeutic drug monitoring may help achieve similar benefits as dual therapy.

In the section of colon cancer, the authors provide useful data that current treatments lower this risk substantially. It is notable that more recent reports suggest that there have been improvements in the rates of colon cancer associated with IBD.

Overall, the section on lymphoma is very good.

In the section on other complications, the presentation suggests that there may be impaired wound-healing with anti-TNFs. I think this risk is overstated in this slide. Also, I think the risk of severe infection with thiopurines is a little bit higher than stated; though, this can be mitigated with careful monitoring.

I think this summary slide could be improved by noting that the overall risk of serious cancers is likely lowered by treating IBD. Since colon cancer is a fairly common cancer and IBD treatment reduces the risk, this likely outweighs the increased risk of other cancers (eg. lymphoma) which are much less common.
Another link to video: https://tinyurl.com/IBDTreatments
Related posts:
Disclaimer: This blog, gutsandgrowth, assumes no responsibility for any use or operation of any method, product, instruction, concept or idea contained in the material herein or for any injury or damage to persons or property (whether products liability, negligence or otherwise) resulting from such use or operation. These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. Because of rapid advances in the medical sciences, the gutsandgrowth blog cautions that independent verification should be made of diagnosis and drug dosages. The reader is solely responsible for the conduct of any suggested test or procedure. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.