A Chandra, M Shepard. NEJM 2025; 393: 833-835. The Corporatization Deal — Health Care, Investors, and the Profit Priority
The authors of this article have a sanguine interpretation of the health care landscape. Here are some excerpts:
The health care industry is exceptional in the United States: it relies on private businesses operating in markets to fulfill a fundamental human need. Because of health care’s essential nature, many observers have viewed the growing influence of large companies in the industry, known as “corporatization,” as odious, akin to privatization of fire and police departments. The corporatization of health care often evokes images of rapacious companies that prioritize profits over patients, since corporations operate according to the logic of business, emphasizing efficiency and financial returns, whereas medical institutions have traditionally operated as professional or charitable enterprises…
Evaluating corporatization requires understanding why it occurs, when it can succeed, and why it can go wrong.
Corporatization represents a deal between organizations and investors. New technologies, upgraded facilities, research and development, and competitive salaries are expensive but are necessary to meet the expectations of patients, who value improvements in health more than improvements in other goods. Investors supply the capital needed to support these enhancements and, in exchange, expect a financial return on their investment….Corporatization unlocks capital in return for growth that prioritizes profits, and investors may take an ownership stake in an organization or adjust management incentives to generate the necessary profits.
But is this deal a good one?…agreements are voluntary and therefore presumably benefit the investors and medical organizations involved. But the key question for society and for policymakers is whether corporatization benefits groups that are not party to such deals: patients and payers…
But for several reasons, health care is exceptional among U.S. markets in that profits and value often don’t align.
First, patients may not be able to accurately assess the quality of medical care, so firms can make money by cutting corners, with little fear of affecting demand. Second, firms may engage in corporatization simply to build market power, which drives up prices. Third, many medical products and services are fundamentally unprofitable because people who could benefit from them cannot afford them…
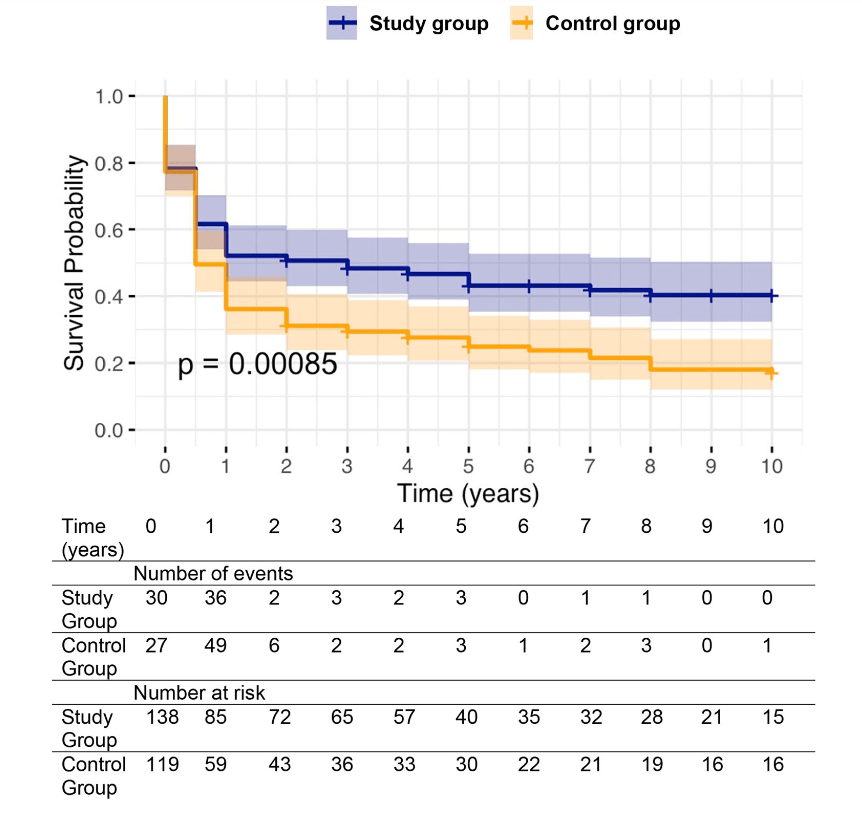
Corporatization’s effects on nursing home care appear to be largely negative. After being acquired by a private equity firm, nursing homes tend to avoid sicker residents, deliver lower-quality care, and have higher resident mortality2 …
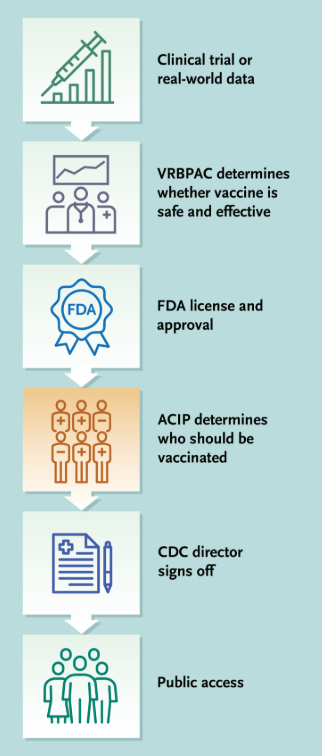
The biopharmaceutical industry is an example of a sector that probably couldn’t exist without investors, since enormous amounts of funding are needed to conduct expensive clinical trials with high failure rates…
Corporatization isn’t the only tool medical firms can use to raise capital. One alternative is government funding, including subsidized loans or tax credits. But relying on public financing has downsides. Governments struggle to identify what patients want, owing to bureaucratic hurdles, a lack of incentives, and budgetary constraints. They are also subject to shifting political climates, making them unreliable funders for large or long-term investments that require steady outlays…
What steps can be taken to unlock the benefits of corporatization while limiting its harms? The guiding objective should be better aligning profits (which drive corporate decision making) with value for patients…
A second approach involves empowering regulators to enforce antitrust rules aimed at limiting market power that wasn’t sanctioned — or regulating prices when those efforts fail. But regulators already have these goals and struggle to achieve them because of tight budgets and bureaucratic limits…
Corporatization will always involve trade-offs because there is no simple or universal “fix” to align profits with value for patients. In each area of medicine, regulators will need to decide whether the deal inherent to corporatization is a worthwhile one — and whether the alternatives are any better.
My take: It is refreshing to see a different viewpoint regarding the profit-driven U.S. health care system. While this is not the system most observers would have created, it is what we have and the currently available alternatives could be worse.
Related blog posts:
- Unpacking Health Care Corporatization in the U.S.
- “The Broken Promises of Profit-Driven Medicine”
- ‘Physicians Are Not the Victims’ (Plus One)
- “Commercial Insurance Isn’t in the Health Care Business. It’s in the Financial Business.”
- Healthcare: “Where the Frauds Are Legal”
- No One Would Design U.S. Healthcare System This Way
- NY Times: America can afford a world-class health system. Why don’t we have one?
- We are Last in Health Care Among High Income Countries
- How Insurance Companies Save Millions in Denying Care
- Stopping Insurance Coverage in the Middle of Your Procedure
- Longevity Gap Present Even in Wealthy Americans
- Ten Americas: Examining Health Disparities and Life Expectancy
- The Guardian: UnitedHealth Secretly Paid Nursing Homes to Reduce Hospital Transfers
- NY Times: ‘What’s My Life Worth?’ The Big Business of Denying Medical Care
- High Rates of Denying Medical Care for Medicaid Patients Managed by Health Insurers
- Mark Cuban: Disrupting American Healthcare
Plants at the Chicago Botanic Garden: