Yesterday’s notes highlighted the most useful discussion at this year’s meeting regarding mucosal healing (MH) in inflammatory bowel disease.
Many points were intriguing but often at odds. For example, the speakers noted that symptoms and scoring systems like CDAI are unreliable in establishing remission. It was noted that the FDA is mandating more objective measures (like endoscopic improvement) in future studies. Yet, the studies cited for their arguments often were derived from studies which did not use objective endpoints. Similarly, some of the arguments were based on small studies and yet experts often caution to use evidence-based medicine.
Bo Shen (Cleveland Clinic) “Surgerical Options in IBD”
- 50-71% of CD patients require some type of surgery within 10 years of diagnosis
- End-ileostomy may be a cure for some CD patients, For UC, end-ileostomy 98% are cured. 2% develop enteritis.
- Can use infliximab after surgery. Immune system different after surgery and may work even
- ‘Don’t operate until a CD patient develops a complication. But, don’t wait until further complications develop.’
Different type strictures –web-like strictures are suitable for dilatation, others are more difficult: spindle-like (longer) , ulcerated stricture, and anastomotic.
- Classification: Gast Endosc 2013; 78: 8181-35.
- Etiology: primary, secondary (anastomotic), benign, malignant
- Short-long: Length (<4cm) if dilating
- Degree: high-grade, low-grade
- Number: single, multiple
- Associated conditions: abscess, others
Determining resection margin –does not depends on absence of histologic activity (Ann Surg 1996; 224: 563-71). Try to save as much bowel as possible, often based on how thick bowel is rather than histologic margins.
Save the gut –stricturoplasty. 1st surgery –usually is a resection rather than stricture plasty. Heineke-Mikulicz (most common) <10 cm for short , Finney for strictures 10-20 cm, Michelassi >20 cm (sid-to-side isoperistaltic). (Dis Colon Rectum 2007) Stricturoplasty –best for mid small bowel, minimum inflammation, no fistula
Fistula –Hollow-organ to hollow-organ fistula –treat surgically. Whereas if fistula is perianal, start with medical treatment. Perianal fistulas often treated with seton; seton often kept in place for a long time (“forever if not bothering patient”).
Abscess—avoid surgical drainage if possible. Delineate anatomy and consider elective surgery later. If less than 3 cm, could aspirate and not leave in drain. If >3 cm, start with interventional radiology
Post-op management –Ruttgerts score. Rescope 6 months post-op to determine if needs more aggressive treatment.
UC Surgery: issues: preoperative biologics, 2- or 3-stage operations, what type of pouch
- There may be increased risk with biologics (studies have not shown this consistently) –depends on type of surgery. If very sick, use 3-stage rather than 2-stage operation. Don’t do pouch at time of 1st operation if very sick DCR 2013; 56: 1243-52).
- J-pouch now standard. Kock pouch –catheterize pouch/no ostomy. S-pouch –problemswith mechanical obstruction.
- Even with mucosectomy (vs. stapler/no mucosectomy)–can still develop cuffitis and malignancy. Mucosectomy may increase risk of incontinence.
Edward Loftus (Mayo Clinic) “Optimizing Biologic Therapy: Maximizing Benefit and Minimizing Risk”
Is azathioprine an effective drug? Should we be using biologics sooner?
Key points:
- ACT1 and ACT2 were pivotal studies for infliximab approval for UC. 1/3rd chance of going into full remission, 1/3rd chance of response, 1/3rd chance of not responding. Infliximab lowers risk of colectomy. Favorable studies of other anti-TNFs as well: adalimumab (Gastroenterol 2012; 142: 257-65) and golimumab (Gastroenterol 2014; 46: 85-95 & 96-109). No head-to-head anti-TNF trials.
- Crohn disease: 5-ASA products don’t work for Crohn disease. Reviewed pivotal trials of anti-TNF agents (infliximab, adalimumab, certolizumab)-30% in remission.
- Natalizumab (anti-alpha 4 integrin) for refractory disease was discussed (NEJM 2005; 353: 1912-25). Takes longer to work then anti-TNFs but maintenance data look good. PML risk: 395 cases among 118,100 patients treated as of August 2013. Lots of paperwork and physicians have to be certified. If you are JC virus serology is negative, “your risk is about 1 in one million in the next year. If you are positive, about a 1% risk in the following year.”
- Azathioprine (AZA) not very effective (Gastroenterol 2013; 145: 766-74 & 758-65). Prospective double-blind Spanish study (n=131) –no statitistical benefit. 2nd reference is French study. N=132. No significant difference at 36 months in patients with added AZA. In U.S., most “thought leaders” going straight to anti-TNFs.
- Combination therapy works best in adults (SONIC study for Crohn disease, UC Success for UC). UC Success only studied 16 weeks, no maintenance therapy trial. However, methotrexate (MTX) with anti-TNFs combination has not been proven to be effective (Gastroenterol 2014; 146: 681-8). Reason this was a negative study, per lead author, may have been related to steroid use.
Other pointers:
- Don’t rely on symptoms alone. Symptoms/CDAI do not correlate with CDEIS (endoscopic improvement). FDA mandating all future trials have an endoscopic endpoint and not rely on use of CDAI alone. Other factors cause symptoms including IBS, infections, and bacterial overgrowth. Take-home point: Need to look (endoscopy) if someone is not doing well.
- In the SONIC trial –if there was inflammation on endoscopy, there was an impressive 30% delta in response to treatment (with combination therapy compared with AZA monotherapy). Whereas if you have no lesions, combination therapy no more effective than either monotherapy agent. Patients whose complaints are due to irritable bowel rather than inflammation do not respond well to treatment.
- OLD paradigm –treat based on symptoms. NEW paradigm–treat based on biologic/radiographic markers or endoscopic findings. “Treat to target” has been approach used by Dr. Sandborn. Target mucosal healing and then assess mucosal healing every 6 months until target achieved, then less frequently. Yet mucosal healing cannot be achieved in many/most patients.
- Therapeutic drug monitoring. For example, 6-TGN >235 associated with better response to AZA (OR 5.0)
- Pharmacokinetics of anti-TNFs: lower clearance if concomitant use of immunomodulators, increased clearance if high CRP, higher BMI
- New drugs: Ustekinumab –three phase 3 trials underway. Should be available in about 2 yrs for Crohn disease. Vedolizumab –under FDA review (NEJM 2013; 369: 699-710). Infusion (similar to remicade frequency). Blocks lymphocyte homing in the gut. UC data much more robust than with CD, but probably will be approved for both. Rate of adverse events were low. Etrolizumab—similar to Vedolizumab, but SC administered. Currently, this drug is in phase 2 studies.
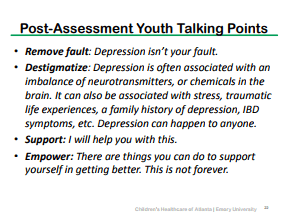
Eva Szigethy (Pittsburgh Pediatrics) “Psychological evaluation and assessment in IBD”
Key points:
- Anxiety/depression ~25-40% of pediatric IBD. Occurs in both active and inactive disease.
- IBD effects on brain: inflammation, drugs (steroids, biologics)–both have direct effects on brain.
- 15% of kids and 25% of adults are having thoughts of death on screening tools. Pain is frequent trigger for suicidal thoughts.
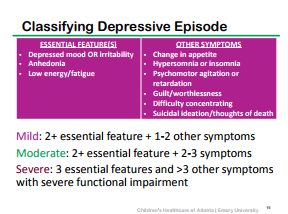
- Simple depression screen: Mood, Energy, Sleep, Suicide/Self-esteem, Anhedonia (lack of pleaure), Guilt, Eating (change in appetite)
- We should not ignore adjustment disorders. We may be able to prevent a full-blown psychiatric disorder. Each time we let problems like anxiety or depression go untreated, this can leave long-term changes in brain.
- Anxiety screen: Tense, Tired, Recurrent worries/fear, Restless, Avoidance, Poor sleep/nightmares, Poor concentration
- Important to look at patient perspective of their disease: identity (what they see as their symptoms), cause/etiology, timeline (how long the patient believes that the illness will last), consequences, cure/control.
- Catastrophizing –more persistent pain and increased visceral hyperalgesia. Abnormal brain activation. Poor coping drives development of depression and anxiety.
- With adult IBD, 20% of patients consume up to 80% of medical costs. Chronic pain and depression are key factors (Binion et al 2010).
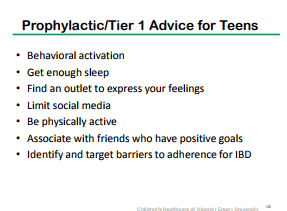
- Management of anxiety/depression: Cognitive Behavioral therapy –changing behaviors and thinking, problem-solving. ACT –activities, calm (relaxation, guided imagery, hypnosis), think positive (cognitive reframing). Antidepressants: TCA, SSRI, SNRI. SSRI/SNRI –few side effects or drug interactions. Overdose risk is highest with TCA (but typically using low doses of these agents). No pediatric studies in IBD and only small studies in adults. If inactive IBD, SSRI often 1st line. If active IBD, Bupropion often used as 1st line.
- For anxiety, most likely use SSRI if comorbid anxiety
- For pain, most likely use SNRI or low dose TCA
- Opiates are problematic due to psychological/physical dependence, increased mortality/infection risk, narcotic bowel
- Sleep –don’t go to bed if not tired, aim for consistency, if not asleep in 20 minutes, then do something else. 1st line pharmacology: consider antihistamines or melatonin.
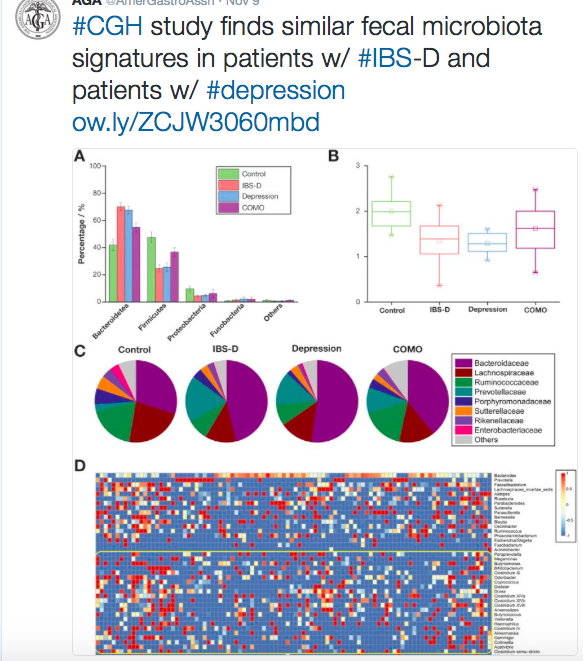
Sachin Kunde (Michigan State University, Helen DeVos Children’s Hospital) “FMT for IBD”
Key points:
- Microbial diversity altered in IBD –can we modulate dysbiosis to treat IBD?
- Issues with cause and effect. Is dysbiosis due to IBD or causing IBD.
- FMT –“the ultimate probiotic.” Application of FMT. For recurrent C difficile, cure rate nearly 90% –?better with lower GI route. For any indication besides C difficile infection (CDI), can only be given through clinical trials (FDA IND). Currently 9 ongoing trials for IBD (1 pediatric, 3 in U.S).
FMT in IBD: Studies:
- -Anderson et al. Aliment Phar Ther 2012: 13/18 without CDI had some resolution of IBD symptoms.
- -Kunde et al JPGN 2013: n=10. PUCAI decrease by 15 indicated response found in 78% (7/9) at 1 week, and 67% (6/9) at 1 month, 3 (33%) went into remission.
- -Kump et al IBD 2013: n=6. FMT for UC was not effective. Transient improvement in 2/6 patients, 1/6 improved on Mayo sub score.
Bottomline for FMT & IBD: More questions than answers: efficacy, route of administration, # of infusions needed, fresh vs. frozen, adverse effects, best donor, etc.
For today’s post today and yesterday’s post, I may have made some transcription errors and these notes were not reviewed with the speakers. Also, due to brevity, some useful information was not included. Thus, the disclaimer with these posts is particularly important.
Disclaimer: These blog posts are for educational purposes only. Specific dosing of medications (along with potential adverse effects) should be confirmed by prescribing physician. This content is not a substitute for medical advice, diagnosis or treatment provided by a qualified healthcare provider. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a condition.
Related blog posts: