I wanted to congratulate/recognize this year’s awardees at NASPGHAN and to summarize some of the associated presentations.
This blog entry has abbreviated/summarized the presentations. Though not intentional, some important material is likely to have been omitted; in addition, transcription errors are possible as well.
Major Awards:
- Harry Shwachman Award: Peter Whitington (Children’s Hospital of Chicago) This award is given for major life long scientific contribution to the field of pediatric gastroenterology.
- Distinguished Service Award: Melvin Heyman (UCSF Division Chief and JPGN editor). This award is given for excellence and service in the field of pediatric gastroenterology.
- AAP Murray Davidson Award: Jeffrey Hyams (Division Chief Connecticut Children’s)This award is given to an outstanding clinician, scientist and educator.
Fellow Research Award: “Bile Acid Signatures in Children Confer Protection From Clostridium Difficil Infection” ME Tessier et al (Baylor College of Medicine). Conclusions: Stool bile acids profiles are different in children with C difficile infection and could be a predisposing factor. C diff toxins may alter bile acid profiles via inducing epithelial FGF-19 production.
Young Investigator Award “Analysis of Candidate Genes by Whole Exome Sequencing in Very Early-Onset IBD” J Kelsen (CHOP), et al. VEO-IBD cohort. Excellent presentation! (Related blog post: Just the Beginning: Mutations in Very Early Onset ..)
- Children <5 years/extensive controls.
- Mutation Findings: IL10RA/IL21R variants, RAG2/PIK3R1 variants
- Presentation included phenotypic description (clinical and immunity/functional analysis)
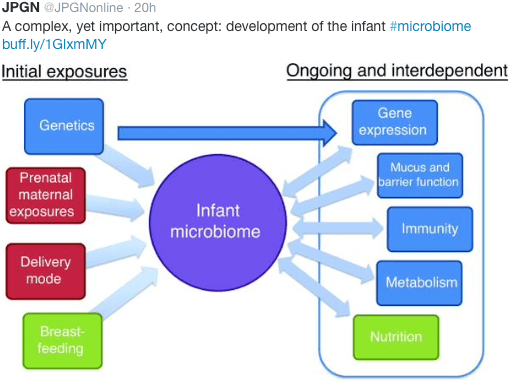
- Gut microbiome development being studied as well
- Trying to combine microbiome data with genomic data.
William Balistreri Prize “A Prospective Newborn Screening Study for Biliary Atresia” Sanjiv Harpavat (Baylor College of Medicine) et al. Excellent talk!
Background: 67 infants with biliary atresia (2007-2014) on retrospective review—ALL had elevated conjugated/direct bilirubin levels in first 24-48 hours of life. (Related blog post: Diagnosing biliary atresia earlier | gutsandgrowth)
Repeat testing at 2 weeks can identify those infants that need to be followed closely. Workup needed for those who remained abnormal at 2 weeks of life.
This algorithm was studied at 4 different hospitals in Houston with 2-12% premature infants)
In newborn period:
- N=11,636 –121 abnormal on newborn testing (based on hospital’s normative values -usually direct bilirubin >0.4)
- When repeated at 2 weeks: 102 of these 121 were normal/only 12 continued to test high (2 with BA, 1 A1AT, 1 Rh disease, 8 resolved). The two patients detected with biliary atresia is in line with the expected frequency of ~1 in 5000.
- 7 missed retesting. 3 died (congenital heart disease), 2 missed followup, 2 had PCP refuse retesting.
- Testing results: 100% sensitivity. Good specificity with repeat testing.
Baylor Workup approach to cholestasis:
- 3-4 day evaluation
- Day 1: liver panel, A1AT typing, U/S, CXR
- Days 2-4: liver biopsy/percutaneous cholangiogram, +/- Kasai
Current AAP recommendation (per Ronald Sokol) is for all infants to have fractionated bilirubin.
Take-home message: How can we diagnose every infant on time? Possibly check every infant for direct/conjugated bilirubin in first 48 hours.
Young Clinical Investigator Award: “Poop-MD: A mobile health application accurately identifies acholic stools.” Douglas Mogul
Problem of delayed diagnosis has been improved in some studies with stool color cards. With emergence of smart phones (80% of 18-35 year olds have smart phones), opportunity to identify echoic stools with new technology.
- PoopMD. Software determines whether stool is bloody, acholic, etc. Can email doctor and place reminder. FREE app.
- Parents takes the picture of stool and then app analyzes.
- Pilot study with 45 initial photographs reviewed by panel of 7 pediatricians
- When at least 6 physicians agreed on stool color as being acholic (n=7), this was tested against app
- App: 100% sensitivity for acholic stools. 89% specificity.
- Working on Spanish version and improved interface.
Other awards:

NASPGHAN Foundation Awards

Sponsored Awards