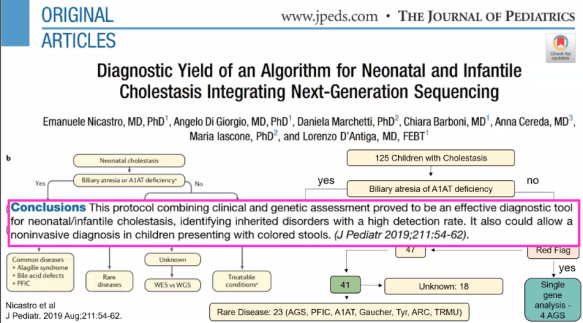
S Harpavat et al. JAMA 2020; 323: 1141-50. Link: Diagnostic Yield of Newborn Screening for Biliary Atresia Using Direct or Conjugated Bilirubin Measurements
This article provides details on how to improve the outcomes of children with biliary atresia by detecting cases at an earlier age. The authors provide details on their 2-stage approach at near-universal screening of 124,385 infants in South Texas/Texas Medical Center from 2015-2018 and compare their results to a prior cohort.
Methods: The authors sought to have all infants have a fractionated bilirubin within the first 60 hours of life. This information can easily be obtained due to preexisting policy of testing total bilirubin in this time-frame. Those with any abnormal direct bilirubin or conjugated bilirubin had a 2nd stage screening at 2 weeks of life. At stage 2, any infant with a direct bilirubin >1 mg/dL or higher than 1st stage were considered abnormal. The stage 2 screening aligned with AAP-recommended 2 week check up. During the screening time-frame (2015-2018), 7 patients were identified with BA (one treated at outside institution), 7 more from nonstudy hospitals who had replicated protocol, and 6 referred due to clinical symptoms.
Key findings:
- 7 infants with biliary atresia were detected with 100% sensitivity and 100% NPV. The PPV was 5.9% and specificity was 99.9%. Due to the small number of infants identified, the confidence limits for sensitivity was 56%-100%.
- During the first stage, 1354 infants (1.1%) had abnormal values. At stage 2, 119 had abnormal values (0.1% of initial cohort and 8.9% of those with 1st stage abnormalities).
- Range of direct/conjugated bilirubins in those with eventual biliary atresia: Stage 1 —0.4-2.3,and Stage 2 —1.6-3.5
- In the 2015-2018 time-frame, age at time of Kasai was lowered from 56 days to 36 days, P=.004.
- The actual time between presentation to specialist to time of Kasai was unchanged ~12 days.
- In the 2015-18 time-frame, 11 of 19 (58%) had Kasai at less than 30 days (optimal timing) compared to 3 of 24 in historical cohort.
- Many (n=53) other cholestatic conditions were identified in the stage 2 cohort. 52.7% of abnormal stage 2 tests had no diagnosis determined.
- Nine had cholestatic diseases: Alagille (n=4), A1AT (n=3), ABCB11 (n=1), Choledochal cyst (n=1).
- Twelve were heterozygous for a liver disease.
- Seventeen had conditions associated with neonatal cholestasis: Trisomy 21 (n=5), Trisomy 18 (n=3), portosystemic shunt (n=2), maternal lupus, omphalocele, and panhypopituitarism.
- Eight had infections including CMV (n=3), and syphilis (n=3). Seven had excessive red blood cell turnover.
- Many of those with abnormal stage 2 evaluations required minimal workup. Additional fractionated bilirubin alone were needed for 28 (25%).
- Premature infants were more likely to have abnormal screening.
- Transplant-free survival at 1 year was greater in cohort during screening period: 94.7% vs. 70.8% with historical cohort (this did not reach statistical significance)
Discussion:
- This 2-stage approach is much more promising than stool color cards. These cards have shown some modest success in countries like Japan and Taiwan which have a national call center and standard 1-month checkups; however, even in these countries, age at time of Kasai were 60 days and 46 days respectively.
- “The challenge specialists [and pediatricians] face was highlighted by an infant who had a true positive screening result in the study, but underwent the Kasai portoenterostomy at 75 days.”
- The cost-effectiveness of this approach is unclear.
My take: The best chance for transplant-free survival in biliary atresia involves establishing an early diagnosis. This study shows one way to accomplish this goal -nothing else has worked despite more than 30 years of trying.
Related blog posts:
- Online Aspen Webinar (Part 5) Biliary Atresia Diagnosis and Screening
- More Data, More Nuance with MMP-7: Best Biliary Atresia Biomarker
- Helpful Review on Biliary Atresia | gutsandgrowth
- Guideline Links: Infant Cholestasis and Esophageal Atresia-Tracheoesophageal fistula | gutsandgrowth
- Bad News Bili | gutsandgrowth
- Stool color cards -Not flashy but effective
- Newborn Bilirubin Measurements To Identify Biliary Atresia | gutsandgrowth
- Outcome of “Successful” Biliary Atresia Patients
- High Survival Rates for Biliary Atresia Patients Needing Liver Transplantation
- 30 -Year Outcomes with Biliary Atresia
- Outcomes of successful Biliary Atresia Patients
- Outcomes of Biliary Atresia | gutsandgrowth