I am happy to say that this is the last nightcall that I will have this year!
Today, I’ve compiled some of my favorite posts from the past year. I started this blog a little more than 10 years ago. I am grateful for the encouragement/suggestions from many people to help make this blog better. Also, I want to wish everyone a Happy New Year.
GI:
- Must-Read: How to Handle Post-Procedure Fevers
- Pictographic Constipation Action Plans
- Carlo DiLorenzo: Lessons Learnt Over 30 Years
- Why Observational Studies Are Misleading and PPI Association with Kidney Stones
- Does It Makes Sense to Look for Celiac Disease in Children with Constipation?
- Secondary Prophylaxis of Clostridiodes difficile Infection
- Pelvic AnoRectal Care Program (PARC)
IBD:
- Expert Consensus: New Recommendations for Therapeutic Drug Monitoring
- Unpacking the Pivotal Ozanimod (True North) Trial
- The Really Simplified Endoscopy Scoring
LIVER:
- Algorithm for Neonatal Acute Liver Failure
- NASPGHAN Alagille Syndrome Webinar
- Aspen Webinar 2021 Part 8 -Neonatal Cholestasis
- Aspen Webinar 2021 Part 2 -Nonalcoholic Steatohepatitis
- Aspen Webinar 2021 Part 1-COVID-19 and the Liver
- Oral Pan-Genotypic HCV Drugs Approved For Children Starting at Age 3 Years
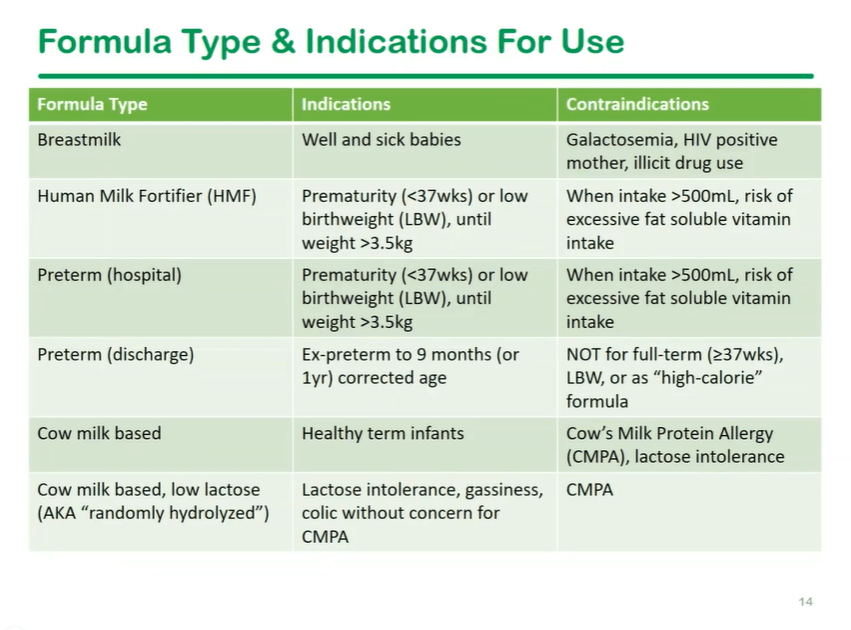
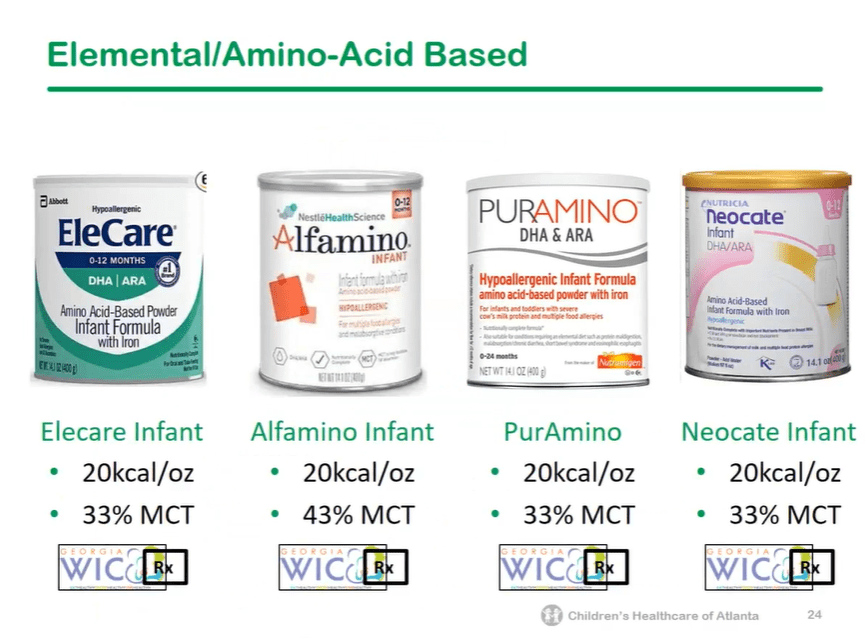
Nutrition:
Other Topics: